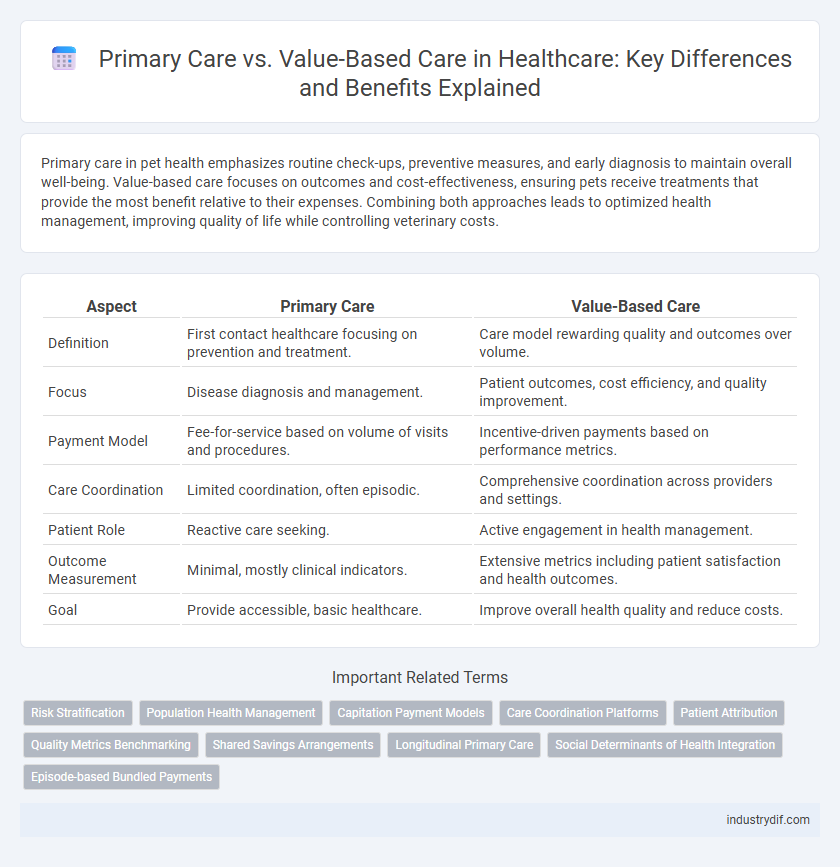
Primary care in pet health emphasizes routine check-ups, preventive measures, and early diagnosis to maintain overall well-being. Value-based care focuses on outcomes and cost-effectiveness, ensuring pets receive treatments that provide the most benefit relative to their expenses. Combining both approaches leads to optimized health management, improving quality of life while controlling veterinary costs.
Table of Comparison
| Aspect | Primary Care | Value-Based Care |
|---|---|---|
| Definition | First contact healthcare focusing on prevention and treatment. | Care model rewarding quality and outcomes over volume. |
| Focus | Disease diagnosis and management. | Patient outcomes, cost efficiency, and quality improvement. |
| Payment Model | Fee-for-service based on volume of visits and procedures. | Incentive-driven payments based on performance metrics. |
| Care Coordination | Limited coordination, often episodic. | Comprehensive coordination across providers and settings. |
| Patient Role | Reactive care seeking. | Active engagement in health management. |
| Outcome Measurement | Minimal, mostly clinical indicators. | Extensive metrics including patient satisfaction and health outcomes. |
| Goal | Provide accessible, basic healthcare. | Improve overall health quality and reduce costs. |
Understanding Primary Care: Definition and Scope
Primary care serves as the first point of contact within the healthcare system, delivering comprehensive, accessible, and continuous care for a broad range of health issues. It encompasses preventive services, diagnosis, treatment of acute and chronic illnesses, and health education. Understanding its scope is essential to distinguish traditional fee-for-service models from value-based care approaches that emphasize quality, patient outcomes, and cost-efficiency.
What Is Value-Based Care? Key Concepts Explained
Value-based care is a healthcare delivery model that prioritizes patient outcomes over the volume of services provided, aiming to improve quality while reducing costs. It focuses on coordinated care, preventive measures, and evidence-based treatments to enhance overall health and reduce hospital readmissions. Key concepts include risk-sharing agreements, performance metrics, and patient-centered approaches that align incentives for providers and payers to achieve better health results.
Core Differences Between Primary Care and Value-Based Care
Primary care centers on providing comprehensive, patient-focused services including prevention, diagnosis, and treatment of common illnesses, ensuring continuity and coordination of care. Value-based care emphasizes outcomes and cost-efficiency, incentivizing healthcare providers to improve patient health through quality metrics and reduced hospital readmissions. The core difference lies in primary care's focus on direct patient interaction versus value-based care's systemic approach to enhancing performance and healthcare value.
Roles of Primary Care Physicians in Patient Management
Primary care physicians serve as the central coordinators in patient management, emphasizing comprehensive care, preventive services, and chronic disease monitoring in both traditional and value-based care models. In value-based care, their role extends to optimizing health outcomes through data-driven decision-making, patient engagement, and care coordination across multidisciplinary teams. These physicians enhance healthcare quality by reducing hospital admissions and improving patient satisfaction, directly influencing cost-efficiency and population health metrics.
Value-Based Care Models: Types and Structures
Value-based care models prioritize patient outcomes by linking healthcare provider payments to the quality and efficiency of care delivered, incorporating structures such as Accountable Care Organizations (ACOs), Patient-Centered Medical Homes (PCMH), and bundled payment systems. ACOs coordinate care across multiple providers to reduce costs and improve health, while PCMH emphasizes continuous, comprehensive primary care centered on patient needs. Bundled payments offer a single, predetermined reimbursement for an entire episode of care, incentivizing providers to avoid unnecessary services and focus on value.
Patient Outcomes: Comparing Primary and Value-Based Approaches
Value-based care prioritizes patient outcomes by incentivizing healthcare providers to deliver high-quality, efficient services that reduce hospital readmissions and improve chronic disease management, contrasting with traditional primary care models focused primarily on service volume. Evidence shows value-based approaches lead to better patient satisfaction, enhanced preventive care, and lower overall healthcare costs due to coordinated treatment plans and outcome-driven protocols. Integrating value-based care strategies within primary care frameworks results in improved clinical results by aligning provider compensation with measurable health improvements.
Financial Implications: Fee-for-Service vs Value-Based Payment
Fee-for-service (FFS) payment models incentivize volume by reimbursing providers for each individual service, often leading to higher healthcare costs without necessarily improving patient outcomes. Value-based care (VBC) shifts the focus to quality and efficiency, rewarding providers for achieving better health outcomes and cost savings, thereby reducing unnecessary treatments and hospital readmissions. Transitioning from FFS to VBC requires investment in data analytics and care coordination but ultimately aligns financial incentives with patient-centered care, promoting sustainable healthcare spending.
Impact on Chronic Disease Management
Primary care serves as the frontline for managing chronic diseases by providing continuous, comprehensive care and fostering strong patient-provider relationships essential for early detection and ongoing management. Value-based care shifts the focus from volume to quality, incentivizing healthcare providers to improve patient outcomes through coordinated care, preventive measures, and efficient resource utilization. This approach leads to better control of chronic conditions such as diabetes and hypertension, reducing hospital readmissions and overall healthcare costs.
Patient Experience: Accessibility and Quality of Care
Primary care emphasizes continuous, personalized patient relationships that improve accessibility through routine check-ups and preventive services. Value-based care enhances quality by incentivizing healthcare providers to deliver outcomes-focused treatments, reducing hospital readmissions and medical errors. Both models prioritize patient experience by ensuring timely access to care and promoting effective health management tailored to individual needs.
Future Trends in Primary Care and Value-Based Care Integration
Future trends in primary care emphasize the integration of value-based care models to enhance patient outcomes and reduce healthcare costs. Embracing technologies like telehealth, data analytics, and personalized medicine enables providers to focus on preventive care and chronic disease management. Health systems increasingly prioritize coordinated care networks, incentivizing quality and efficiency through value-based payment structures.
Related Important Terms
Risk Stratification
Primary care utilizes risk stratification to categorize patients based on health status and potential complications, enabling targeted interventions that improve outcomes and reduce costs. Value-based care integrates risk stratification to allocate resources efficiently, prioritize high-risk populations, and incentivize providers to deliver quality care aligned with patient needs.
Population Health Management
Population Health Management in primary care emphasizes proactive, data-driven strategies to improve health outcomes across diverse populations by addressing social determinants and chronic disease prevention. Value-Based Care aligns financial incentives with quality metrics, rewarding providers for enhancing patient experiences, reducing hospital readmissions, and controlling costs within population health frameworks.
Capitation Payment Models
Capitation payment models in primary care provide a fixed amount per patient regardless of services rendered, incentivizing providers to focus on preventive care and efficient resource use. This value-based care approach aligns financial incentives with patient outcomes, reducing unnecessary treatments and lowering overall healthcare costs.
Care Coordination Platforms
Care coordination platforms integrate patient data across multiple providers to enhance communication and streamline primary care delivery, directly supporting value-based care models by improving outcomes and reducing costs. These platforms enable real-time information sharing, facilitating proactive management of chronic conditions and ensuring patients receive timely, efficient care aligned with value-based incentives.
Patient Attribution
Patient attribution in primary care involves identifying and assigning patients to specific providers to ensure continuity and personalized care, while value-based care emphasizes attributing patients based on quality outcomes and cost-effective management. Accurate patient attribution is critical for measuring provider performance, improving health outcomes, and optimizing reimbursement models within value-based care frameworks.
Quality Metrics Benchmarking
Primary care focuses on comprehensive patient-centered services while value-based care emphasizes quality metrics benchmarking to improve health outcomes and cost efficiency. Quality metrics benchmarking in value-based care involves measuring clinical performance indicators, patient satisfaction, and care coordination to drive accountability and enhance primary care delivery.
Shared Savings Arrangements
Shared Savings Arrangements in primary care incentivize providers to reduce healthcare costs while maintaining quality by sharing the financial benefits resulting from efficient care delivery. This value-based care model aligns provider goals with patient outcomes, promoting preventive care and chronic disease management to avoid costly hospitalizations.
Longitudinal Primary Care
Longitudinal primary care emphasizes continuous patient-provider relationships, improving chronic disease management and preventive care outcomes compared to episodic treatment models. Integrating value-based care principles enhances this approach by incentivizing quality over quantity, reducing hospitalizations, and lowering overall healthcare costs.
Social Determinants of Health Integration
Primary care increasingly integrates social determinants of health (SDOH) to address patients' holistic needs, enhancing care quality and outcomes. Value-based care models prioritize SDOH integration by incentivizing providers to improve population health and reduce healthcare costs through targeted community resources and support services.
Episode-based Bundled Payments
Episode-based bundled payments align with value-based care by providing a fixed reimbursement for an entire treatment episode, incentivizing primary care providers to coordinate services efficiently and improve patient outcomes. This model contrasts with traditional primary care fee-for-service approaches by promoting cost containment and quality metrics across the continuum of care.
Primary Care vs Value-Based Care Infographic
 industrydif.com
industrydif.com