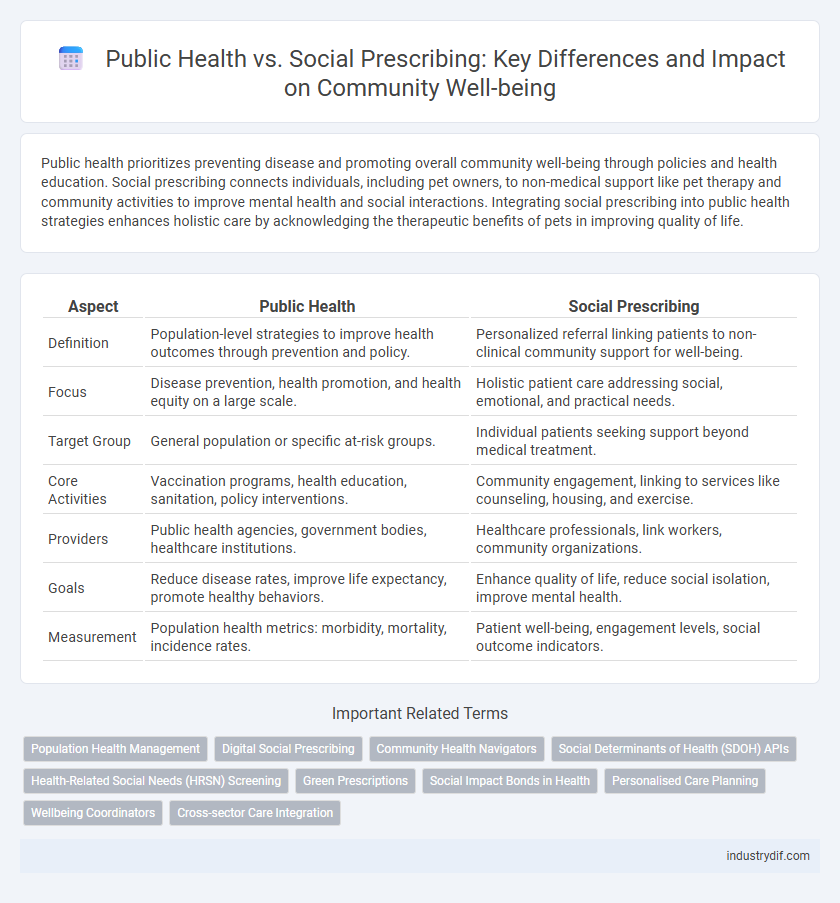
Public health prioritizes preventing disease and promoting overall community well-being through policies and health education. Social prescribing connects individuals, including pet owners, to non-medical support like pet therapy and community activities to improve mental health and social interactions. Integrating social prescribing into public health strategies enhances holistic care by acknowledging the therapeutic benefits of pets in improving quality of life.
Table of Comparison
| Aspect | Public Health | Social Prescribing |
|---|---|---|
| Definition | Population-level strategies to improve health outcomes through prevention and policy. | Personalized referral linking patients to non-clinical community support for well-being. |
| Focus | Disease prevention, health promotion, and health equity on a large scale. | Holistic patient care addressing social, emotional, and practical needs. |
| Target Group | General population or specific at-risk groups. | Individual patients seeking support beyond medical treatment. |
| Core Activities | Vaccination programs, health education, sanitation, policy interventions. | Community engagement, linking to services like counseling, housing, and exercise. |
| Providers | Public health agencies, government bodies, healthcare institutions. | Healthcare professionals, link workers, community organizations. |
| Goals | Reduce disease rates, improve life expectancy, promote healthy behaviors. | Enhance quality of life, reduce social isolation, improve mental health. |
| Measurement | Population health metrics: morbidity, mortality, incidence rates. | Patient well-being, engagement levels, social outcome indicators. |
Understanding Public Health: Definition and Scope
Public health encompasses the organized efforts and informed choices of society, organizations, and individuals aimed at preventing disease, prolonging life, and promoting health through collective actions. Its scope includes monitoring health status, diagnosing community health problems, educating the public, and developing policies to address environmental, social, and economic factors. Unlike social prescribing, which focuses on personalized non-clinical interventions to improve individual well-being, public health operates at a broader population level to improve health outcomes and reduce health disparities.
What is Social Prescribing? Key Concepts Explained
Social prescribing is a holistic approach in public health that connects patients with non-medical resources to improve well-being, such as community groups, physical activities, or counseling services. It addresses social determinants of health by promoting personalized support tailored to individual needs, reducing the burden on healthcare systems. This innovative model enhances patient engagement and contributes to better mental, emotional, and physical health outcomes.
Core Objectives: Public Health vs Social Prescribing
Public Health focuses on preventing disease and promoting health at a population level through policies, education, and surveillance systems designed to reduce health disparities and improve overall community well-being. Social Prescribing aims to connect individuals to non-clinical services, addressing social determinants of health by linking patients with community resources like exercise groups, social clubs, or counseling to improve mental and physical health outcomes. Both approaches share the core objective of enhancing health equity but differ in scale and method, with Public Health targeting systemic changes and Social Prescribing delivering tailored, person-centered support.
Population-Level Impact: How Public Health Shapes Communities
Public health initiatives prioritize disease prevention, health promotion, and equitable access to healthcare services, directly influencing population-level health outcomes and reducing disparities. Social prescribing complements this by linking individuals to community resources, enhancing social well-being and addressing non-medical determinants of health. Together, these approaches foster resilient communities with improved overall health and reduced healthcare burdens.
Personalization in Care: The Role of Social Prescribing
Social prescribing enhances public health by personalizing care through tailored non-medical interventions that address individual social, emotional, and practical needs. It connects patients with community resources such as exercise programs, counseling, and social groups, which traditional healthcare models may overlook. This personalized approach reduces healthcare utilization and improves overall well-being by targeting the root causes of health issues.
Intervention Strategies: Policies vs Person-Centered Approaches
Public health intervention strategies emphasize broad policies such as vaccination programs, sanitation regulations, and health education campaigns to reduce disease risk at the population level. Social prescribing prioritizes person-centered approaches by connecting individuals with community resources like exercise groups, counseling, and social activities to improve mental and physical well-being. Integrating policy-driven public health measures with social prescribing enables a more holistic, effective approach to health promotion and disease prevention.
Collaboration Across Sectors: Integrating Public Health and Social Prescribing
Collaboration across sectors enhances public health outcomes by integrating social prescribing with traditional healthcare services, fostering a holistic approach to patient well-being. Multidisciplinary partnerships between healthcare providers, social services, and community organizations facilitate tailored interventions that address social determinants of health, such as housing, nutrition, and mental health support. This integrated model improves population health equity by connecting individuals to non-clinical resources that complement medical treatment and promote sustainable lifestyle changes.
Measuring Outcomes: Evaluation and Effectiveness
Measuring outcomes in public health and social prescribing involves assessing both population health metrics and individual well-being improvements through validated tools, such as quality of life scales and healthcare utilization data. Evaluation frameworks often integrate quantitative data like hospitalization rates with qualitative feedback from patients to capture the comprehensive impact of interventions. Effectiveness is determined by reductions in health disparities, enhanced patient engagement, and sustained behavior changes that contribute to long-term public health goals.
Barriers and Challenges in Practice
Public health initiatives often face barriers such as limited funding, workforce shortages, and insufficient community engagement that hinder widespread implementation. Social prescribing encounters challenges including lack of awareness among healthcare professionals, variable access to community resources, and difficulties in measuring outcomes effectively. Addressing these obstacles requires integrated strategies to enhance collaboration between healthcare providers, social services, and community organizations.
Future Trends: Bridging Public Health and Social Prescribing
Emerging trends in public health emphasize integrating social prescribing to address broader determinants of health by connecting patients with community resources for holistic care. Data-driven approaches and digital platforms enhance the coordination between healthcare providers and social services, promoting preventive care and reducing healthcare disparities. Future models focus on collaborative frameworks that leverage social prescribing as a critical component to improve population health outcomes and sustainability.
Related Important Terms
Population Health Management
Public health emphasizes large-scale disease prevention and health promotion through policies and community interventions targeting diverse populations. Social prescribing enhances population health management by connecting individuals to non-clinical services, addressing social determinants and improving overall well-being.
Digital Social Prescribing
Digital social prescribing leverages technology to connect patients with non-clinical services like community activities and support groups, enhancing traditional public health strategies by addressing social determinants of health. This approach improves access, streamlines referrals, and promotes holistic well-being through personalized, digitally-enabled interventions.
Community Health Navigators
Community Health Navigators play a crucial role in bridging Public Health initiatives with Social Prescribing by connecting individuals to non-clinical services that address social determinants of health. This approach enhances holistic well-being by integrating personalized support within community settings, thereby improving access to resources and reducing health inequities.
Social Determinants of Health (SDOH) APIs
Social Determinants of Health (SDOH) APIs enable the integration of critical social and environmental data into healthcare systems, enhancing social prescribing by personalizing interventions based on factors like housing, education, and economic stability. These APIs support public health initiatives by facilitating real-time data exchange, improving population health management, and addressing health inequities through targeted social care referrals.
Health-Related Social Needs (HRSN) Screening
Health-Related Social Needs (HRSN) screening serves as a critical tool in public health by identifying social determinants affecting individual well-being, whereas social prescribing connects patients to community resources addressing those identified needs. Integrating HRSN screening within social prescribing frameworks enhances care outcomes by systematically targeting underlying social factors contributing to health disparities.
Green Prescriptions
Green prescriptions in public health encourage patients to engage in nature-based activities to improve mental and physical well-being, reducing reliance on pharmaceutical treatments. Social prescribing integrates these green prescriptions as a holistic approach, linking healthcare with community resources to address social determinants of health effectively.
Social Impact Bonds in Health
Social Impact Bonds (SIBs) in health leverage private investment to fund preventative public health initiatives, enabling social prescribing programs that address social determinants of health like loneliness and chronic conditions. This financing model aligns investor returns with health outcomes, promoting cost-effective interventions that reduce healthcare demand and improve population well-being.
Personalised Care Planning
Personalised care planning in public health emphasizes tailored interventions to improve individual outcomes, while social prescribing integrates non-clinical support such as community activities to address holistic health needs. Both approaches enhance patient engagement and wellbeing by aligning medical treatment with social and lifestyle factors, driving more effective, patient-centered care strategies.
Wellbeing Coordinators
Wellbeing Coordinators play a crucial role in bridging public health initiatives and social prescribing by connecting individuals to community resources that enhance holistic health outcomes. Their expertise in tailoring personalized support plans improves mental and physical wellbeing, reducing healthcare system burdens and promoting sustained community engagement.
Cross-sector Care Integration
Public health initiatives emphasize broad community health improvements through policy, education, and prevention strategies, while social prescribing integrates cross-sector care by linking patients to non-clinical services addressing social determinants of health. Effective cross-sector care integration bridges healthcare, social services, and community resources to enhance holistic patient outcomes and reduce healthcare disparities.
Public Health vs Social Prescribing Infographic
 industrydif.com
industrydif.com