Health Information Exchange (HIE) enables the secure sharing of pet health records across different veterinary providers, improving coordinated care and reducing errors. Data liquidity in pet health refers to the seamless access, transfer, and usability of this data in real-time, enhancing decision-making and treatment outcomes. Prioritizing both HIE and data liquidity ensures comprehensive, timely, and accurate pet health management.
Table of Comparison
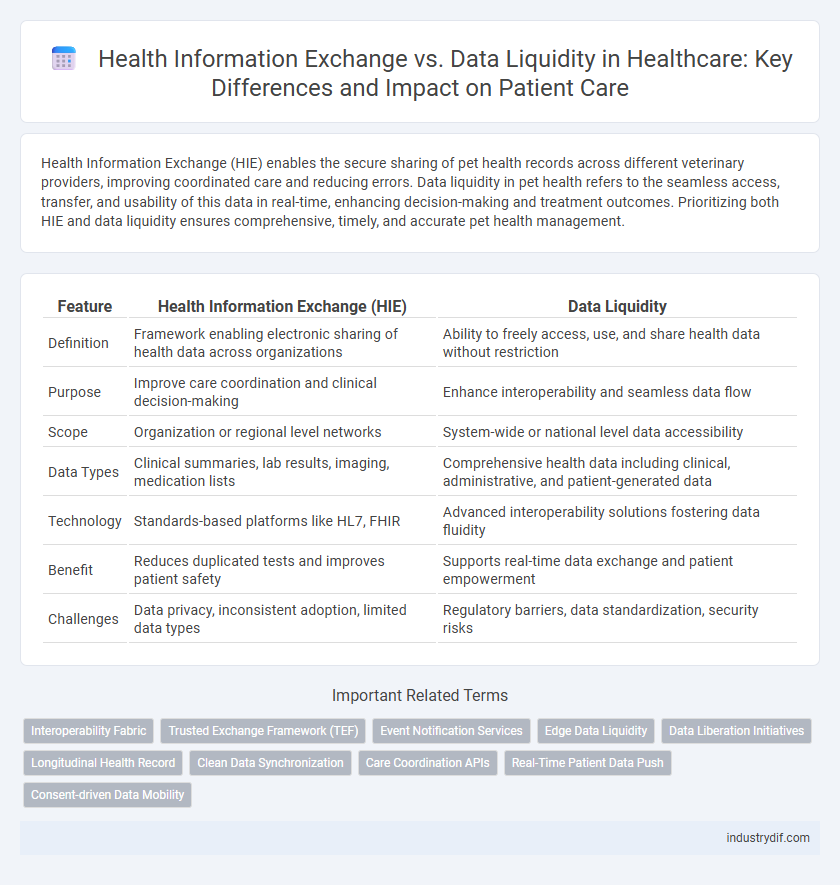
| Feature | Health Information Exchange (HIE) | Data Liquidity |
|---|---|---|
| Definition | Framework enabling electronic sharing of health data across organizations | Ability to freely access, use, and share health data without restriction |
| Purpose | Improve care coordination and clinical decision-making | Enhance interoperability and seamless data flow |
| Scope | Organization or regional level networks | System-wide or national level data accessibility |
| Data Types | Clinical summaries, lab results, imaging, medication lists | Comprehensive health data including clinical, administrative, and patient-generated data |
| Technology | Standards-based platforms like HL7, FHIR | Advanced interoperability solutions fostering data fluidity |
| Benefit | Reduces duplicated tests and improves patient safety | Supports real-time data exchange and patient empowerment |
| Challenges | Data privacy, inconsistent adoption, limited data types | Regulatory barriers, data standardization, security risks |
Understanding Health Information Exchange (HIE)
Health Information Exchange (HIE) enables the secure sharing of patient data across different healthcare organizations, enhancing care coordination and reducing duplication of tests. Unlike data liquidity, which emphasizes seamless access and usability of health data across systems, HIE focuses on establishing standardized protocols and trusted networks for data exchange. Optimizing HIE infrastructure improves interoperability, supporting more accurate clinical decision-making and better patient outcomes.
Defining Data Liquidity in Healthcare
Data liquidity in healthcare refers to the seamless, secure, and efficient flow of patient information across various health systems, enabling real-time access to accurate clinical data. Unlike traditional Health Information Exchange (HIE) models that often involve complex data standards and limited interoperability, data liquidity emphasizes minimizing barriers to data sharing, ensuring that critical health information is available when and where it is needed. Enhanced data liquidity supports improved care coordination, reduces duplicative testing, and drives better patient outcomes by fostering a more connected and responsive healthcare ecosystem.
Key Differences Between HIE and Data Liquidity
Health Information Exchange (HIE) enables the secure sharing of patient data across different healthcare organizations to improve care coordination, whereas data liquidity emphasizes the seamless flow and accessibility of health information for real-time clinical decision-making. HIE often involves standardized protocols and centralized platforms to facilitate information exchange, while data liquidity focuses on interoperable systems and minimizing data silos for quick retrieval and use. The primary difference lies in HIE's role as an infrastructure for data sharing versus data liquidity's focus on the dynamic and continuous availability of actionable health data.
Importance of Seamless Data Flow in Healthcare
Seamless data flow in healthcare enhances patient outcomes by enabling real-time access to critical health information across providers, reducing errors and duplication of tests. Health Information Exchange (HIE) systems facilitate structured communication between entities, while data liquidity ensures continuous, unrestricted movement of data to support clinical decisions and patient care coordination. Optimizing interoperability standards like FHIR promotes efficient data sharing, improving care quality and operational efficiency in healthcare networks.
Interoperability Challenges in HIE Systems
Health Information Exchange (HIE) systems face significant interoperability challenges due to disparate data standards and inconsistent implementation of protocols across healthcare providers, hindering seamless data sharing. Data liquidity within HIE requires real-time, accurate exchange of patient information, yet system fragmentation and lack of standardized terminologies like HL7 FHIR limit effective interoperability. Addressing these challenges involves adopting universal healthcare data standards and enhancing API-based integrations to improve clinical data accessibility and support coordinated patient care.
Advantages of High Data Liquidity for Providers
High data liquidity enables healthcare providers to access and share patient information seamlessly across multiple systems, improving care coordination and reducing duplicate testing. Enhanced data flow supports timely clinical decisions, leading to better patient outcomes and operational efficiencies. Providers benefit from streamlined workflows and comprehensive data insights that foster proactive treatment strategies.
Regulatory Impacts on Health Data Exchange
Health Information Exchange (HIE) frameworks are heavily influenced by regulatory policies such as HIPAA and the 21st Century Cures Act, which mandate strict privacy and interoperability standards to ensure secure patient data sharing. Data liquidity emphasizes seamless and real-time access to health information, but regulatory constraints often limit data availability and require compliance with consent management and audit requirements. Effective navigation of these regulations is essential for achieving both robust data liquidity and secure, compliant health data exchange across healthcare systems.
Role of Standards in Facilitating Data Liquidity
Standards like HL7 FHIR and CDA play a crucial role in facilitating data liquidity by enabling seamless Health Information Exchange (HIE) across disparate healthcare systems. These standardized protocols ensure interoperability, allowing real-time access, sharing, and integration of patient data among providers, payers, and patients. Effective adoption of these standards reduces data silos, promotes accurate clinical decision-making, and enhances care coordination.
Privacy and Security Considerations
Health Information Exchange (HIE) enables the secure sharing of patient data across different healthcare organizations, prioritizing privacy through encryption and strict access controls. Data liquidity emphasizes the seamless and timely availability of health data but requires robust security frameworks to prevent unauthorized access and ensure compliance with HIPAA regulations. Balancing data liquidity with privacy safeguards is crucial to protect patient confidentiality while supporting efficient clinical decision-making.
Future Trends in Health Data Exchange and Liquidity
Future trends in health data exchange emphasize the enhancement of interoperability frameworks and the adoption of standardized APIs to improve data liquidity across diverse health systems. Advances in blockchain technology and artificial intelligence enable secure, real-time sharing and analysis of comprehensive patient data, promoting personalized medicine and population health management. Regulatory support for data portability and patient consent mechanisms further accelerates seamless integration and dynamic accessibility of health information nationwide.
Related Important Terms
Interoperability Fabric
Health Information Exchange (HIE) enables the secure sharing of patient data across disparate healthcare systems, while Data Liquidity emphasizes seamless accessibility and usability of health data. An Interoperability Fabric acts as a dynamic framework, integrating diverse data sources to facilitate real-time exchange and enhance clinical decision-making efficiency.
Trusted Exchange Framework (TEF)
The Trusted Exchange Framework (TEF) establishes standardized protocols to enhance Health Information Exchange (HIE) by ensuring secure, interoperable data sharing across disparate systems, addressing critical barriers to data liquidity in healthcare. TEF's role is pivotal in enabling seamless patient data access and improving clinical decision-making through reliable, consent-based information flows.
Event Notification Services
Event Notification Services within Health Information Exchange (HIE) systems enhance data liquidity by enabling real-time alerts about patient encounters, test results, and care transitions across healthcare providers. These services facilitate seamless clinical workflow integration, reduce redundant testing, and improve patient outcomes by ensuring critical health data flows promptly to authorized users.
Edge Data Liquidity
Edge Data Liquidity enhances Health Information Exchange by enabling real-time, secure access and sharing of patient data at the point of care, improving clinical decision-making and outcomes. This approach optimizes interoperability across disparate health systems, ensuring seamless data flow while maintaining privacy and compliance standards.
Data Liberation Initiatives
Data liberation initiatives in health information exchange focus on enhancing data liquidity by enabling seamless, interoperable access to patient records across diverse healthcare systems, thus improving care coordination and patient outcomes. These initiatives promote standardized protocols and open APIs to break down data silos, ensuring real-time, secure sharing of comprehensive health information.
Longitudinal Health Record
Health Information Exchange (HIE) enables the secure sharing of patient data across different healthcare systems, facilitating a comprehensive Longitudinal Health Record (LHR) that captures a patient's medical history over time. Data Liquidity ensures this clinical information flows seamlessly and in real-time, enhancing care coordination, reducing redundant tests, and improving patient outcomes through up-to-date, accessible longitudinal records.
Clean Data Synchronization
Health Information Exchange (HIE) enables seamless Clean Data Synchronization across diverse healthcare systems by standardizing patient records and reducing errors. Data Liquidity emphasizes the timely, secure flow of accurate health information, facilitating coordinated care and improving clinical decision-making.
Care Coordination APIs
Care Coordination APIs enhance Health Information Exchange (HIE) by enabling seamless data liquidity, allowing healthcare providers to access and share patient information in real-time for improved clinical decision-making. These APIs support interoperability standards like FHIR, facilitating coordinated care workflows and reducing redundancies across diverse health systems.
Real-Time Patient Data Push
Health Information Exchange (HIE) enables secure real-time patient data push across healthcare systems, enhancing clinical decision-making and care coordination by providing timely access to comprehensive patient records. Data liquidity emphasizes seamless interoperability and rapid data flow without barriers, ensuring that critical patient information is instantly available to authorized providers when needed for immediate intervention.
Consent-driven Data Mobility
Consent-driven data mobility in Health Information Exchange (HIE) empowers patients to control the sharing of their medical records, ensuring privacy and compliance with regulations like HIPAA. This approach enhances data liquidity by enabling secure, interoperable access to health information across providers while respecting patient preferences and consent directives.
Health Information Exchange vs Data Liquidity Infographic
 industrydif.com
industrydif.com