Personalized medicine in pet health tailors treatments based on an individual animal's genetic profile, lifestyle, and environment, enhancing therapeutic effectiveness. Polygenic risk scoring evaluates multiple genetic variants to predict an animal's susceptibility to complex diseases, guiding preventive care. Integrating these approaches allows veterinarians to optimize health outcomes by combining precise diagnostics with targeted interventions.
Table of Comparison
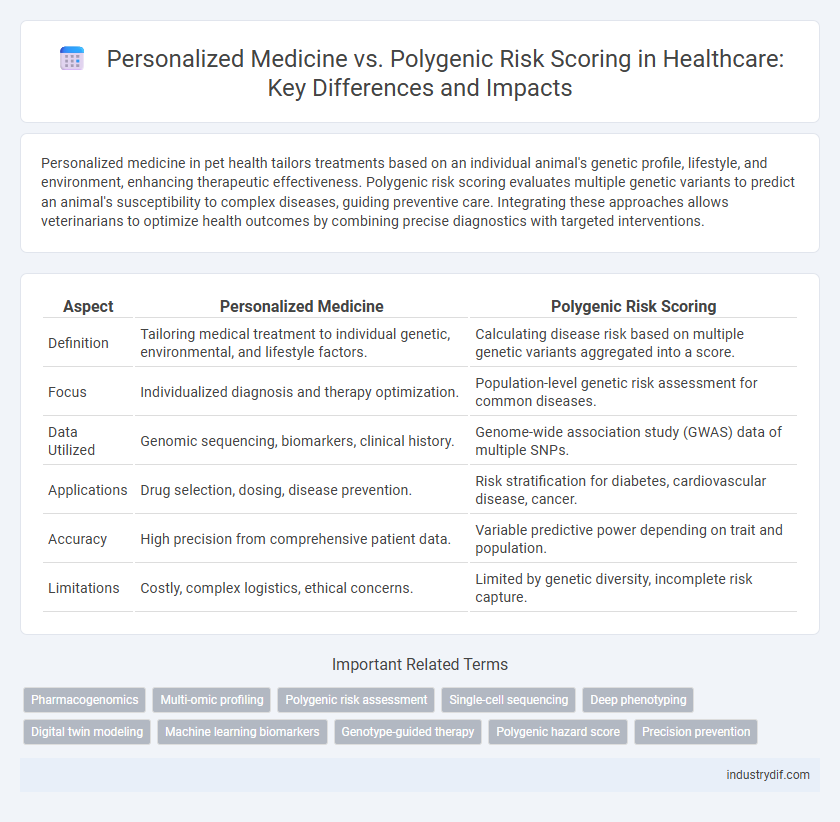
| Aspect | Personalized Medicine | Polygenic Risk Scoring |
|---|---|---|
| Definition | Tailoring medical treatment to individual genetic, environmental, and lifestyle factors. | Calculating disease risk based on multiple genetic variants aggregated into a score. |
| Focus | Individualized diagnosis and therapy optimization. | Population-level genetic risk assessment for common diseases. |
| Data Utilized | Genomic sequencing, biomarkers, clinical history. | Genome-wide association study (GWAS) data of multiple SNPs. |
| Applications | Drug selection, dosing, disease prevention. | Risk stratification for diabetes, cardiovascular disease, cancer. |
| Accuracy | High precision from comprehensive patient data. | Variable predictive power depending on trait and population. |
| Limitations | Costly, complex logistics, ethical concerns. | Limited by genetic diversity, incomplete risk capture. |
Understanding Personalized Medicine in Healthcare
Personalized medicine in healthcare tailors medical treatment to individual genetic, environmental, and lifestyle factors, enhancing diagnostic accuracy and therapeutic effectiveness. Polygenic risk scoring aggregates multiple genetic variants to estimate an individual's predisposition to complex diseases, contributing valuable data for personalized risk assessment. Integrating polygenic risk scores into personalized medicine enables proactive disease prevention and optimized patient-specific interventions.
Defining Polygenic Risk Scoring
Polygenic risk scoring quantifies an individual's genetic predisposition to diseases by aggregating the effects of numerous genetic variants across the genome. This method enables risk stratification for complex diseases such as cardiovascular conditions, diabetes, and various cancers, enhancing the precision of predictive models. Unlike personalized medicine, which tailors treatment to individual characteristics, polygenic risk scoring focuses on genetic risk prediction to inform preventative strategies.
How Personalized Medicine Differs from Polygenic Risk Scoring
Personalized medicine tailors medical treatment to an individual's unique genetic makeup, lifestyle, and environmental factors for precise healthcare interventions. Polygenic risk scoring estimates an individual's genetic predisposition to certain diseases by analyzing the combined effect of multiple genetic variants. Unlike personalized medicine's comprehensive approach, polygenic risk scoring primarily focuses on genetic risk prediction without integrating environmental or lifestyle data.
Clinical Applications of Personalized Medicine
Personalized medicine revolutionizes clinical practice by tailoring treatments based on individual genetic profiles, improving drug efficacy and minimizing adverse effects. Polygenic risk scoring complements this approach by quantifying the cumulative effect of multiple genetic variants, enhancing disease prediction and prevention strategies. These tools enable clinicians to design targeted interventions for complex diseases like cancer, cardiovascular disorders, and diabetes, optimizing patient outcomes through precision healthcare.
Genetic Insights: The Role of Polygenic Risk Scores
Polygenic risk scores aggregate the effects of multiple genetic variants to quantify an individual's genetic predisposition to complex diseases, offering a more comprehensive genetic insight than personalized medicine approaches that often focus on single-gene mutations. These scores enable clinicians to stratify patients based on genetic risk, improving disease prediction and prevention strategies for conditions like heart disease, diabetes, and certain cancers. Integration of polygenic risk scoring into personalized medicine enhances precision health by tailoring interventions to the combined influence of numerous genetic factors rather than isolated genetic markers.
Advantages and Limitations of Personalized Medicine
Personalized medicine offers tailored treatment plans based on an individual's unique genetic makeup, improving drug efficacy and reducing adverse effects. Its advantages include precise diagnostic insights and targeted therapies that enhance patient outcomes, yet limitations involve high costs, complex data interpretation, and limited accessibility in clinical settings. While personalized medicine excels in individualized care, challenges such as ethical concerns and the need for extensive genomic data integration persist.
Strengths and Challenges of Polygenic Risk Scoring
Polygenic risk scoring (PRS) leverages genetic data from thousands of variants to estimate an individual's predisposition to complex diseases, offering a more comprehensive risk assessment compared to single-gene analyses. Its strengths include the ability to quantify cumulative genetic risk for conditions like coronary artery disease, diabetes, and certain cancers, enabling earlier interventions and personalized prevention strategies. Challenges involve the need for diverse population data to improve prediction accuracy and the integration of PRS with environmental and lifestyle factors to enhance clinical utility.
Integration of Genetic Data in Healthcare Decision-Making
Personalized medicine leverages comprehensive genetic profiles to tailor treatment plans for individual patients, enhancing therapeutic efficacy and minimizing adverse effects. Polygenic risk scoring aggregates multiple genetic variants to predict susceptibility to complex diseases, informing preventive healthcare strategies. Integrating these genetic tools into healthcare decision-making optimizes patient outcomes by combining risk prediction with customized interventions.
Future Trends: Combining Personalized Medicine and Polygenic Risk Scoring
Future trends in healthcare emphasize the integration of personalized medicine with polygenic risk scoring to enhance disease prediction and prevention strategies. By leveraging genomic data and individual health profiles, clinicians can develop tailored treatment plans that improve patient outcomes and reduce adverse effects. Advances in AI and machine learning are accelerating the ability to analyze complex genetic information alongside environmental factors, enabling more precise and dynamic healthcare solutions.
Ethical and Privacy Concerns in Genomic Healthcare
Personalized medicine leverages individual genetic information to tailor treatments, raising ethical issues related to informed consent and equitable access. Polygenic risk scoring aggregates multiple genetic variants to predict disease susceptibility, intensifying privacy concerns due to data sharing across platforms and potential misuse by insurers or employers. Both approaches demand stringent regulatory frameworks to protect patient confidentiality and prevent genetic discrimination in healthcare settings.
Related Important Terms
Pharmacogenomics
Pharmacogenomics tailors drug therapies to an individual's genetic makeup, enhancing treatment efficacy and minimizing adverse reactions. Polygenic risk scoring aggregates multiple genetic variants to predict disease susceptibility, supporting personalized medicine by identifying patients who may benefit from targeted pharmacological interventions.
Multi-omic profiling
Multi-omic profiling integrates genomic, transcriptomic, proteomic, and metabolomic data to enhance personalized medicine by providing comprehensive molecular insights for tailored treatment strategies. Polygenic risk scoring quantifies genetic susceptibility to diseases but lacks the multi-dimensional biological context captured through multi-omic approaches, limiting its predictive accuracy compared to personalized medicine driven by multi-omic profiling.
Polygenic risk assessment
Polygenic risk assessment utilizes the analysis of multiple genetic variants to quantify an individual's predisposition to complex diseases, enabling early detection and tailored prevention strategies. This approach enhances personalized medicine by integrating comprehensive genomic data to improve risk prediction beyond single-gene analyses.
Single-cell sequencing
Single-cell sequencing advances personalized medicine by enabling precise analysis of individual cellular genomes, facilitating tailored therapies based on unique genetic profiles. Unlike polygenic risk scoring, which estimates disease risk using aggregated genetic variants, single-cell sequencing uncovers intratumoral heterogeneity and rare cell populations, improving diagnosis and treatment strategies.
Deep phenotyping
Deep phenotyping enhances personalized medicine by providing detailed and precise characterization of individual patient traits, which improves the accuracy of polygenic risk scoring for complex diseases. Integrating comprehensive phenotypic data with genomic information allows for more tailored prevention and treatment strategies, optimizing patient outcomes in clinical practice.
Digital twin modeling
Digital twin modeling integrates personalized medicine and polygenic risk scoring by creating virtual replicas of patients that simulate genetic risk factors and predict individual health outcomes more accurately. This advanced approach enhances precision in treatment planning and early disease detection through continuous data integration and real-time analysis.
Machine learning biomarkers
Machine learning biomarkers enhance personalized medicine by analyzing complex genetic and phenotypic data to tailor treatments for individual patients, whereas polygenic risk scoring aggregates multiple genetic variants to predict disease risk at a population level. Integrating machine learning with polygenic risk scoring improves the precision of disease prognosis and therapeutic strategies by identifying intricate biomarker patterns beyond traditional methods.
Genotype-guided therapy
Genotype-guided therapy tailors medical treatments based on an individual's genetic profile, enhancing drug efficacy and minimizing adverse effects. Polygenic risk scoring aggregates multiple genetic variants to predict disease risk, providing a complementary approach to personalized medicine by informing prevention and early intervention strategies.
Polygenic hazard score
Polygenic hazard score integrates genetic variants to estimate an individual's age-specific risk for complex diseases, enabling more precise risk stratification compared to traditional polygenic risk scoring. This approach enhances personalized medicine by tailoring prevention and intervention strategies based on dynamic genetic risk profiles over time.
Precision prevention
Personalized medicine leverages individual genetic, environmental, and lifestyle data to tailor prevention and treatment plans, enhancing precision prevention outcomes. Polygenic risk scoring quantifies the cumulative effect of multiple genetic variants to predict disease risk, enabling targeted interventions for high-risk individuals within precision prevention strategies.
Personalized medicine vs Polygenic risk scoring Infographic
 industrydif.com
industrydif.com