Vaccination is a critical component of pet health, providing protection against common infectious diseases by stimulating the immune system. mRNA vaccines represent a cutting-edge advancement, offering faster development times and enhanced immune responses without using live pathogens. Both traditional and mRNA vaccines contribute significantly to preventive veterinary medicine, improving pet longevity and quality of life.
Table of Comparison
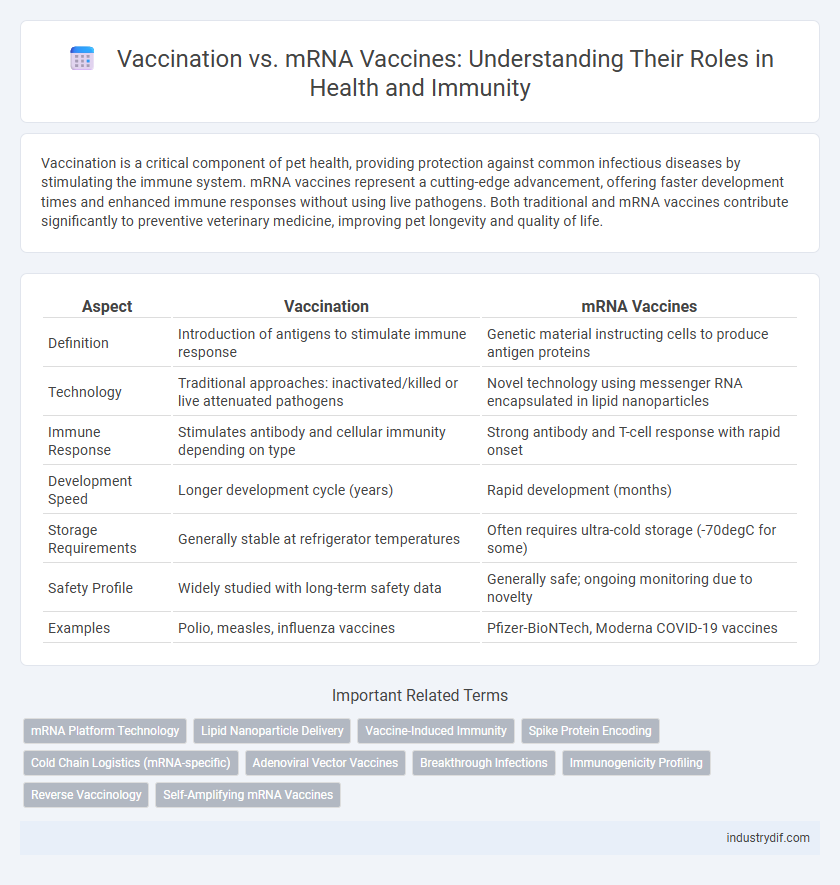
| Aspect | Vaccination | mRNA Vaccines |
|---|---|---|
| Definition | Introduction of antigens to stimulate immune response | Genetic material instructing cells to produce antigen proteins |
| Technology | Traditional approaches: inactivated/killed or live attenuated pathogens | Novel technology using messenger RNA encapsulated in lipid nanoparticles |
| Immune Response | Stimulates antibody and cellular immunity depending on type | Strong antibody and T-cell response with rapid onset |
| Development Speed | Longer development cycle (years) | Rapid development (months) |
| Storage Requirements | Generally stable at refrigerator temperatures | Often requires ultra-cold storage (-70degC for some) |
| Safety Profile | Widely studied with long-term safety data | Generally safe; ongoing monitoring due to novelty |
| Examples | Polio, measles, influenza vaccines | Pfizer-BioNTech, Moderna COVID-19 vaccines |
Understanding Traditional Vaccines: Mechanisms and Applications
Traditional vaccines use weakened or inactivated pathogens to stimulate the immune system, triggering antibody production and long-term immunity. These vaccines have a proven track record in preventing diseases like measles, polio, and influenza by introducing antigens that mimic natural infection. Understanding their mechanisms helps in appreciating their safety, efficacy, and role in global public health vaccination programs.
Introduction to mRNA Vaccines: A New Era in Immunization
mRNA vaccines represent a groundbreaking advancement in immunization by using messenger RNA to instruct cells to produce a protein that triggers an immune response. These vaccines offer rapid development, high efficacy, and adaptability against emerging infectious diseases compared to traditional vaccination methods. Their success in combatting COVID-19 has paved the way for innovative approaches in preventing various viral infections and improving global public health.
Key Differences Between Conventional and mRNA Vaccines
Conventional vaccines typically use weakened or inactivated pathogens to stimulate an immune response, while mRNA vaccines deliver genetic instructions to cells to produce a specific viral protein that triggers immunity. mRNA vaccines can be developed faster and tailored more precisely to emerging variants due to their synthetic production process. Additionally, mRNA vaccines do not contain live virus, reducing the risk of infection compared to some traditional vaccine platforms.
Efficacy Rates: Traditional Vaccines vs mRNA Vaccines
Traditional vaccines, such as inactivated or live-attenuated vaccines, generally show efficacy rates ranging from 50% to 90%, depending on the disease and population. mRNA vaccines, notably those developed for COVID-19, demonstrate higher efficacy rates typically between 90% and 95%, attributed to their precise targeting of viral spike proteins. Comparative studies highlight mRNA vaccines' ability to induce robust immune responses with rapid adaptability to emerging variants, enhancing overall effectiveness.
Safety Profiles: Assessing Adverse Reactions and Risks
Vaccination safety profiles vary between traditional vaccines and mRNA vaccines, with mRNA vaccines showing lower incidences of severe adverse reactions in clinical trials and real-world data. Common side effects of mRNA vaccines include mild to moderate symptoms such as injection site pain, fatigue, and headache, while rare but serious risks like myocarditis have been closely monitored and remain extremely uncommon. Traditional vaccines carry established safety records but may involve different reactogenicity profiles, emphasizing the importance of ongoing pharmacovigilance and risk-benefit analysis in vaccination strategies.
Manufacturing Processes: Traditional Methods vs mRNA Technology
Traditional vaccination manufacturing processes involve cultivating weakened or inactivated pathogens in eggs or cell cultures, a time-consuming method requiring large-scale bioreactors and extensive purification steps. In contrast, mRNA vaccine production utilizes synthetic processes to generate messenger RNA sequences encoding viral antigens, enabling rapid scalability and reduced dependency on biological substrates. This streamlined mRNA technology allows for faster adaptation to emerging variants and more efficient resource utilization compared to conventional vaccine production techniques.
Storage and Distribution Challenges: Comparative Analysis
Vaccination storage and distribution face distinct challenges with traditional vaccines often requiring consistent refrigeration between 2degC and 8degC, whereas mRNA vaccines demand ultra-cold storage conditions as low as -70degC, complicating logistics and limiting accessibility in low-resource settings. The intricate cold chain for mRNA vaccines increases transportation costs and necessitates specialized equipment, whereas traditional vaccines benefit from established infrastructure and broader global distribution networks. Efficient management of these requirements is critical to maximizing vaccine reach and ensuring timely immunization coverage worldwide.
Regulatory Approval for Vaccines: Traditional vs mRNA
Traditional vaccines undergo rigorous regulatory review focused on safety and efficacy through established platforms like live-attenuated or inactivated viruses, often requiring longer clinical trial phases. mRNA vaccines received expedited regulatory approval, leveraging novel technology and adaptive trial designs to address urgent public health needs, while maintaining strict safety evaluations under agencies such as the FDA and EMA. Both vaccine types must meet stringent criteria, but mRNA vaccines benefit from enhanced flexibility in design and rapid manufacturing, influencing regulatory pathways significantly.
Public Perception and Vaccine Hesitancy
Public perception of vaccination has shifted significantly with the introduction of mRNA vaccines, which are often seen as innovative but prompt concerns about long-term effects, fueling vaccine hesitancy. Studies show that misinformation about mRNA technology contributes to skepticism more than traditional vaccine platforms, impacting vaccination rates. Effective public health communication emphasizing the safety and efficacy of mRNA vaccines can address hesitancy and improve overall acceptance.
Future Trends: The Evolving Landscape of Vaccine Development
mRNA vaccine technology is revolutionizing the future of immunization by enabling rapid development and adaptation against emerging infectious diseases. Advanced lipid nanoparticle delivery systems and personalized vaccine designs are expected to improve efficacy and reduce side effects. Predictive genomics and AI-driven platforms are accelerating the identification of novel antigens, shaping next-generation vaccines with broader protection.
Related Important Terms
mRNA Platform Technology
mRNA vaccine platform technology enables rapid development and high efficacy by using messenger RNA to instruct cells to produce specific antigens, triggering a strong immune response without using live virus components. This innovative approach offers scalable manufacturing and adaptability against emerging infectious diseases, revolutionizing traditional vaccination methods.
Lipid Nanoparticle Delivery
Lipid nanoparticle delivery systems enhance mRNA vaccine efficacy by protecting fragile mRNA strands and facilitating targeted cellular uptake, resulting in robust immune responses. Unlike traditional vaccines that introduce weakened pathogens, mRNA vaccines rely on lipid nanoparticles to efficiently transport genetic instructions, accelerating vaccine development and adaptability against emerging infectious diseases.
Vaccine-Induced Immunity
Vaccine-induced immunity from traditional vaccines typically involves exposure to an inactivated or attenuated pathogen, stimulating a broad immune response, while mRNA vaccines deliver genetic instructions for cells to produce a specific viral protein, eliciting a targeted immune reaction. Studies show mRNA vaccines generate strong neutralizing antibodies and T-cell responses, often with quicker development times and adaptability to emerging variants.
Spike Protein Encoding
Vaccination using traditional methods introduces inactivated viruses or protein subunits to trigger immune response, whereas mRNA vaccines deliver genetic instructions encoding the spike protein of SARS-CoV-2, promoting endogenous spike protein production that elicits targeted immunity. This spike protein encoding in mRNA vaccines enables rapid adaptation to viral variants and precise immune system training against COVID-19.
Cold Chain Logistics (mRNA-specific)
Cold chain logistics are critical for mRNA vaccines, requiring ultra-low temperature storage between -80degC and -60degC to maintain vaccine efficacy, unlike traditional vaccines that typically need standard refrigeration. The complexity of this cold chain infrastructure impacts global distribution, necessitating specialized freezers, temperature monitoring systems, and rapid transport solutions to prevent degradation of the sensitive mRNA molecules.
Adenoviral Vector Vaccines
Adenoviral vector vaccines, distinct from traditional vaccination methods and mRNA vaccines, utilize a modified virus to deliver genetic material that stimulates an immune response against specific pathogens. These vaccines are pivotal in pandemic response due to their stability at standard refrigeration temperatures and robust induction of both humoral and cellular immunity.
Breakthrough Infections
Breakthrough infections occur when vaccinated individuals contract COVID-19 despite immunization, highlighting the necessity for ongoing surveillance and booster doses to maintain immunity. mRNA vaccines, such as Pfizer-BioNTech and Moderna, demonstrate high efficacy in reducing severe disease and hospitalization, yet breakthrough cases emphasize the evolving challenge posed by emerging variants.
Immunogenicity Profiling
Vaccination with mRNA vaccines generates robust immunogenicity by stimulating both humoral and cellular immune responses, characterized by strong neutralizing antibody titers and activation of CD4+ and CD8+ T cells. Comparative immunogenicity profiling reveals that mRNA vaccines elicit higher antigen-specific responses and longer-lasting immunity compared to traditional vaccine platforms.
Reverse Vaccinology
Reverse vaccinology leverages genomic data to identify novel vaccine targets, enhancing the development of both traditional vaccines and mRNA vaccines by enabling precise antigen selection. This approach accelerates the creation of mRNA vaccines, optimizing immune responses against pathogens with improved efficacy and safety profiles.
Self-Amplifying mRNA Vaccines
Self-amplifying mRNA vaccines enhance immune response by replicating their RNA inside cells, requiring lower doses compared to conventional mRNA vaccines, which directly introduce mRNA without amplification. This innovative approach improves vaccine efficiency, reduces production costs, and supports faster scalability in immunization programs targeting infectious diseases.
Vaccination vs mRNA Vaccines Infographic
 industrydif.com
industrydif.com