Public health traditionally centers on human health and disease prevention within communities, emphasizing sanitation, vaccination, and epidemic control. One Health expands this focus by integrating human, animal, and environmental health, recognizing the interconnectedness of pet health and zoonotic disease transmission. This holistic approach promotes collaborative efforts across sectors to prevent outbreaks and enhance overall ecosystem well-being.
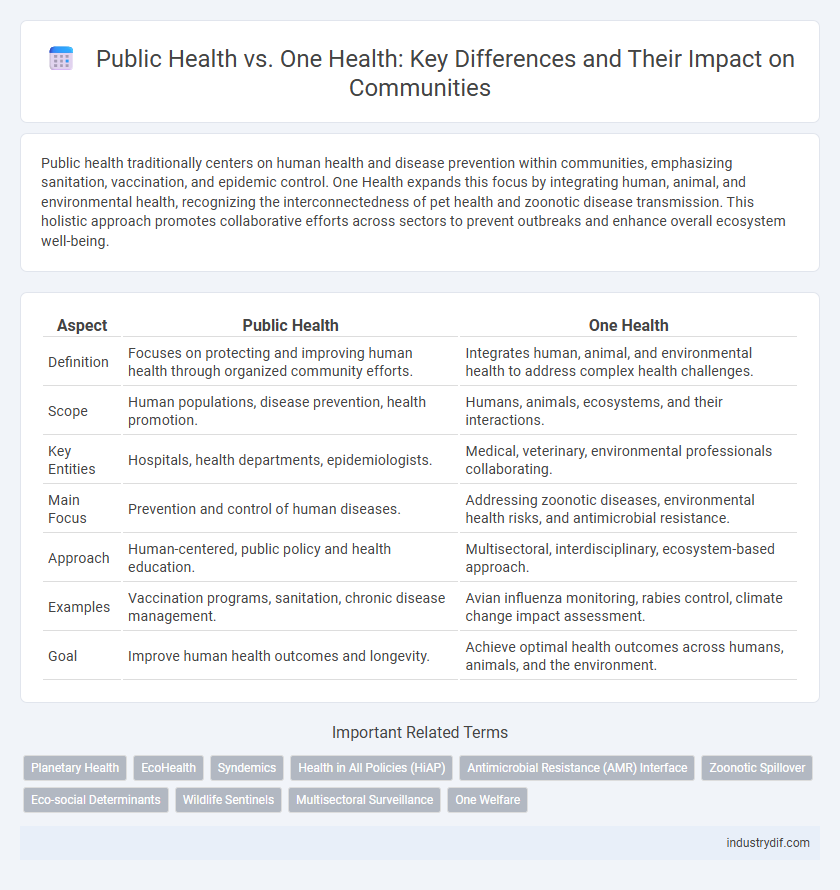
Table of Comparison
| Aspect | Public Health | One Health |
|---|---|---|
| Definition | Focuses on protecting and improving human health through organized community efforts. | Integrates human, animal, and environmental health to address complex health challenges. |
| Scope | Human populations, disease prevention, health promotion. | Humans, animals, ecosystems, and their interactions. |
| Key Entities | Hospitals, health departments, epidemiologists. | Medical, veterinary, environmental professionals collaborating. |
| Main Focus | Prevention and control of human diseases. | Addressing zoonotic diseases, environmental health risks, and antimicrobial resistance. |
| Approach | Human-centered, public policy and health education. | Multisectoral, interdisciplinary, ecosystem-based approach. |
| Examples | Vaccination programs, sanitation, chronic disease management. | Avian influenza monitoring, rabies control, climate change impact assessment. |
| Goal | Improve human health outcomes and longevity. | Achieve optimal health outcomes across humans, animals, and the environment. |
Defining Public Health: Scope and Objectives
Public Health encompasses the prevention of disease, promotion of health, and prolongation of life through organized community efforts, targeting populations rather than individuals. Its scope includes epidemiology, biostatistics, health services administration, environmental health, and health education, aiming to control infectious diseases, improve sanitation, and address social determinants of health. The primary objective of Public Health is to enhance overall community health outcomes by implementing policies and programs that reduce health risks and increase access to care.
Understanding One Health: Integrating Sectors
One Health is an integrative approach linking human, animal, and environmental health to address complex health challenges. This framework promotes collaboration between sectors such as medicine, veterinary science, and environmental science to improve disease prevention and control. Understanding One Health enhances public health strategies by incorporating ecosystem dynamics and zoonotic disease management.
Core Differences Between Public Health and One Health
Public Health primarily targets the prevention of diseases and promotion of health within human populations through organized community efforts and policy interventions. One Health adopts a multidisciplinary approach that integrates human, animal, and environmental health, emphasizing the interconnectedness of these domains to address complex health challenges. The core difference lies in Public Health's exclusive human focus, whereas One Health incorporates animal and ecosystem health to create comprehensive solutions.
Historical Evolution of Public Health and One Health
The historical evolution of public health traces back to ancient sanitation practices, with significant advancements during the 19th century through vaccination and epidemiology, addressing human disease prevention on a population level. One Health emerged in the early 21st century as a multidisciplinary approach integrating human, animal, and environmental health to tackle zoonotic diseases and global health threats. This paradigm shift reflects an evolving understanding that interconnected ecosystems influence disease dynamics, advocating for collaborative efforts among medical, veterinary, and environmental sciences.
Interdisciplinary Approaches in Disease Prevention
Public Health and One Health both emphasize interdisciplinary approaches in disease prevention by integrating expertise from human medicine, veterinary science, and environmental health. This collaboration enhances surveillance systems and outbreak response, addressing zoonotic diseases and environmental factors impacting population health. Coordinated efforts across sectors improve early detection and control of infectious diseases, ultimately promoting comprehensive health security.
Human, Animal, and Environmental Health Interactions
Public Health traditionally focuses on preventing disease and promoting health within human populations through sanitation, vaccination, and health education. One Health expands this scope by emphasizing the interconnectedness of human, animal, and environmental health, recognizing that zoonotic diseases, environmental degradation, and animal health significantly impact human well-being. Collaborative efforts across veterinary medicine, ecology, and human healthcare are essential for effective disease control and sustainable health solutions.
Policy Implications: Public Health vs One Health
Policy implications of Public Health emphasize disease prevention, health promotion, and access to healthcare within human populations, prioritizing resource allocation for hospitals, vaccinations, and health education programs. One Health policies integrate human, animal, and environmental health, promoting interdisciplinary collaboration to address zoonotic diseases, antimicrobial resistance, and ecosystem health through coordinated surveillance, shared data systems, and cross-sectoral regulations. This holistic approach fosters comprehensive risk management and sustainable health outcomes by bridging gaps between medical, veterinary, and environmental policies.
Global Case Studies: Successes and Challenges
Global case studies reveal Public Health initiatives often target specific diseases with vaccination campaigns, while One Health embraces integrated approaches addressing human, animal, and environmental health simultaneously. Successes include the eradication of smallpox and controlling zoonotic diseases like Ebola through coordinated surveillance and response systems. Challenges persist in resource-limited settings, where fragmented efforts and lack of interdisciplinary collaboration hinder effective prevention and control strategies.
Collaborative Strategies for Health Security
Public Health and One Health frameworks emphasize collaborative strategies for enhancing health security through integrated approaches addressing human, animal, and environmental health. Coordinated surveillance systems and data sharing enable early detection and response to emerging infectious diseases, minimizing outbreak risks globally. Cross-sector partnerships involving healthcare, veterinary, and environmental agencies strengthen resilience against health threats by promoting comprehensive policy development and resource allocation.
Future Directions: Bridging Public Health and One Health
Future directions in bridging Public Health and One Health emphasize integrated surveillance systems that monitor human, animal, and environmental health simultaneously to predict and mitigate disease outbreaks effectively. Emphasizing cross-sector collaboration among healthcare, veterinary, and environmental sciences enhances resource sharing and data-driven decision-making for global health threats. Advancements in digital health technologies and genomic epidemiology support early detection and response, ensuring resilient health systems capable of addressing pandemics and antimicrobial resistance through a unified approach.
Related Important Terms
Planetary Health
Planetary Health extends the frameworks of Public Health and One Health by emphasizing the interdependence of human health, animal health, and the Earth's natural systems. This holistic approach addresses global environmental changes, such as climate change, biodiversity loss, and pollution, recognizing their direct impact on disease emergence and population well-being.
EcoHealth
EcoHealth emphasizes the interconnectedness of ecosystem health, wildlife, and human well-being, integrating ecological principles to address emerging infectious diseases within the One Health framework. This approach advances public health by promoting sustainable environmental practices and biodiversity conservation to mitigate health risks at the human-animal-environment interface.
Syndemics
Syndemics highlight the interconnectedness of multiple epidemics influenced by social, environmental, and biological factors, emphasizing the need for integrated approaches in Public Health and One Health frameworks. One Health advances syndemic management by fostering collaboration across human, animal, and environmental health sectors, addressing complex health challenges more effectively than traditional Public Health strategies alone.
Health in All Policies (HiAP)
Health in All Policies (HiAP) integrates public health considerations into policymaking across sectors to address social determinants and improve population health, aligning with the One Health approach that emphasizes interconnected human, animal, and environmental health. Implementing HiAP fosters collaboration between public health professionals and other sectors, enhancing disease prevention and promoting sustainable health outcomes across communities.
Antimicrobial Resistance (AMR) Interface
Antimicrobial Resistance (AMR) represents a critical interface between Public Health and One Health, as resistant pathogens circulate through humans, animals, and the environment. Coordinated surveillance and integrated interventions across these sectors are essential to effectively combat the spread of AMR and safeguard global health.
Zoonotic Spillover
Zoonotic spillover, the transmission of pathogens from animals to humans, represents a critical intersection between Public Health and One Health frameworks, emphasizing integrated approaches to disease surveillance, prevention, and control. One Health promotes collaboration across human, animal, and environmental sectors to mitigate spillover risks, while Public Health focuses on managing human disease outcomes and implementing community-level interventions.
Eco-social Determinants
Public Health primarily addresses human well-being by analyzing eco-social determinants such as socioeconomic status, environmental exposures, and community resources, while One Health integrates these factors across human, animal, and environmental health to understand interconnected risks and promote holistic disease prevention. Both approaches emphasize the importance of sustainable ecosystems and social equity in mitigating health disparities and enhancing population resilience.
Wildlife Sentinels
Wildlife sentinels serve as critical indicators in both Public Health and One Health frameworks by detecting zoonotic pathogens and environmental hazards that threaten human, animal, and ecosystem health. Their monitoring provides early warnings for disease outbreaks, enhancing surveillance systems and promoting integrated responses across multiple health sectors.
Multisectoral Surveillance
Multisectoral surveillance integrates data across human, animal, and environmental health sectors to enhance early detection of infectious diseases, reflecting the One Health approach's emphasis on collaborative action. Public Health traditionally focuses on human disease tracking, whereas One Health expands surveillance networks to include veterinary and ecological data, fostering comprehensive outbreak prevention and response strategies.
One Welfare
One Welfare integrates animal health, human well-being, and environmental sustainability, emphasizing interconnected welfare systems beyond traditional public health frameworks. This approach promotes holistic strategies addressing mental health, food security, and ecosystem balance to achieve comprehensive societal resilience.
Public Health vs One Health Infographic
 industrydif.com
industrydif.com