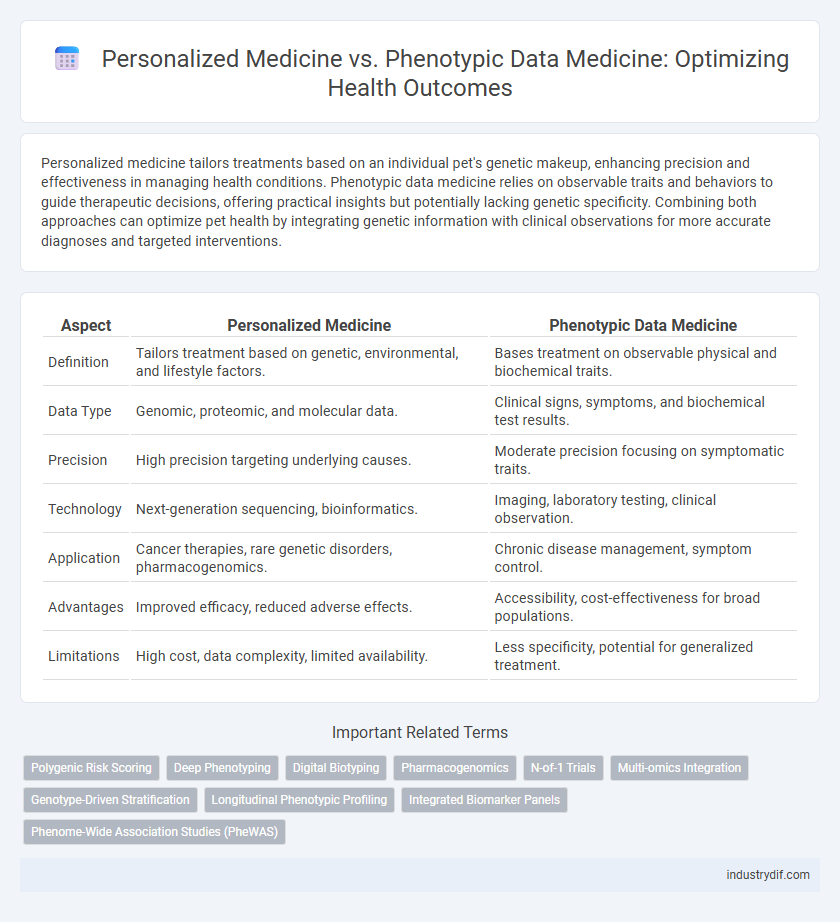
Personalized medicine tailors treatments based on an individual pet's genetic makeup, enhancing precision and effectiveness in managing health conditions. Phenotypic data medicine relies on observable traits and behaviors to guide therapeutic decisions, offering practical insights but potentially lacking genetic specificity. Combining both approaches can optimize pet health by integrating genetic information with clinical observations for more accurate diagnoses and targeted interventions.
Table of Comparison
| Aspect | Personalized Medicine | Phenotypic Data Medicine |
|---|---|---|
| Definition | Tailors treatment based on genetic, environmental, and lifestyle factors. | Bases treatment on observable physical and biochemical traits. |
| Data Type | Genomic, proteomic, and molecular data. | Clinical signs, symptoms, and biochemical test results. |
| Precision | High precision targeting underlying causes. | Moderate precision focusing on symptomatic traits. |
| Technology | Next-generation sequencing, bioinformatics. | Imaging, laboratory testing, clinical observation. |
| Application | Cancer therapies, rare genetic disorders, pharmacogenomics. | Chronic disease management, symptom control. |
| Advantages | Improved efficacy, reduced adverse effects. | Accessibility, cost-effectiveness for broad populations. |
| Limitations | High cost, data complexity, limited availability. | Less specificity, potential for generalized treatment. |
Introduction to Personalized Medicine
Personalized medicine tailors medical treatment to the individual characteristics of each patient, utilizing genetic, environmental, and lifestyle data to optimize therapeutic outcomes. Unlike phenotypic data medicine, which relies primarily on observable traits and symptoms, personalized medicine integrates genomic sequencing, biomarker analysis, and advanced diagnostics to enable precise interventions. This approach improves disease prevention, diagnosis, and treatment by targeting therapies specific to a patient's molecular profile.
Defining Phenotypic Data Medicine
Phenotypic Data Medicine focuses on diagnosing and treating diseases based on observable traits, such as physical characteristics, biochemical markers, and behavioral patterns. This approach leverages comprehensive phenotypic datasets alongside clinical history to tailor therapeutic strategies without relying solely on genetic information. Integrating phenotypic data enhances precision in treatment plans by capturing real-time patient conditions and environmental influences.
Genomic Profiling in Personalized Medicine
Genomic profiling in personalized medicine enables targeted treatment by analyzing individual genetic variations, enhancing drug efficacy and minimizing adverse effects. Unlike phenotypic data medicine, which relies on observable traits and clinical history, genomic profiling offers precise insights into disease mechanisms at the molecular level. Integrating genomic data accelerates the development of customized therapies, significantly improving patient outcomes in oncology, cardiology, and rare genetic disorders.
Role of Phenotypic Data in Clinical Decision-Making
Phenotypic data plays a crucial role in clinical decision-making by providing detailed insights into observable patient characteristics such as physical traits, laboratory results, and lifestyle factors, which complement genetic information in personalized medicine. This data helps clinicians tailor treatments more accurately by addressing real-time health conditions and environmental influences that affect disease progression and drug response. Integrating phenotypic data with genomic profiles enables more precise diagnostics, risk assessments, and therapeutic strategies, enhancing overall patient outcomes in personalized healthcare.
Key Differences Between Personalized and Phenotypic Approaches
Personalized medicine tailors treatment based on individual genetic profiles, leveraging genomic data to predict drug response and disease susceptibility. Phenotypic data medicine relies on observable clinical traits, such as symptoms and biochemical markers, to guide therapy decisions without genetic information. Key differences include personalized medicine's focus on molecular-level data for precision interventions versus phenotypic approaches emphasizing broader physiological manifestations to inform treatment plans.
Benefits of Personalized Medicine for Patient Outcomes
Personalized medicine leverages genetic, environmental, and lifestyle data to tailor treatments specifically to individual patients, resulting in higher efficacy and reduced adverse effects. By targeting therapies based on genetic markers, personalized medicine enhances early diagnosis, optimizes drug response, and prevents disease progression more effectively than phenotypic data medicine. This precision approach improves patient outcomes through customized treatment plans that address the unique biological characteristics of each patient.
Clinical Applications of Phenotypic Data Medicine
Clinical applications of phenotypic data medicine leverage observable traits and patient-specific health information to tailor treatments more accurately than traditional methods. By integrating phenotypic data such as biomarkers, physical characteristics, and lifestyle factors, healthcare providers can enhance diagnostic precision and optimize therapeutic interventions. This approach improves patient outcomes by enabling dynamic adjustments to treatment plans based on real-time phenotypic changes.
Challenges and Limitations of Each Approach
Personalized medicine faces challenges in integrating complex genomic data with clinical practice due to high costs and limited accessibility in diverse populations. Phenotypic data medicine struggles with variability in patient-reported outcomes and the subjective nature of phenotypic observations, which can lead to inconsistent diagnoses. Both approaches require advanced data analytics and standardized protocols to enhance accuracy and clinical utility.
Integration of Genotypic and Phenotypic Data
Integration of genotypic and phenotypic data in personalized medicine enhances diagnostic accuracy by combining genetic information with observable traits, enabling tailored treatment strategies. This approach leverages genomic sequencing alongside clinical phenotypic profiles to predict disease risk, drug response, and therapeutic outcomes more effectively. Advanced bioinformatics platforms facilitate the fusion of these datasets, promoting precision in clinical decision-making and improving patient health management.
Future Trends in Precision Healthcare
Future trends in precision healthcare emphasize the integration of personalized medicine with phenotypic data to enhance diagnostic accuracy and treatment efficacy. Leveraging genomic sequencing combined with real-time phenotypic markers enables tailored therapies that adapt to individual patient variability. Emerging technologies in AI-driven data analysis and wearable biosensors are pivotal in translating phenotypic insights into dynamic, patient-specific care models.
Related Important Terms
Polygenic Risk Scoring
Polygenic Risk Scoring enhances Personalized Medicine by analyzing multiple genetic variants to predict disease susceptibility, enabling tailored prevention and treatment strategies. In contrast, Phenotypic Data Medicine relies on observable traits and clinical data, offering immediate but less precise risk assessments compared to the genetic depth provided by polygenic scoring.
Deep Phenotyping
Deep phenotyping enhances personalized medicine by providing comprehensive phenotypic data, enabling precise treatment tailored to individual genetic, environmental, and lifestyle factors. Integrating high-resolution phenotypic profiles with genomic information improves diagnostic accuracy and optimizes therapeutic strategies in clinical practice.
Digital Biotyping
Digital biotyping enhances personalized medicine by integrating phenotypic data with genomic and proteomic information, enabling precise patient-specific diagnostics and targeted therapies. This approach leverages advanced algorithms and wearable devices to continuously collect and analyze phenotypic markers, improving disease prediction and treatment customization beyond traditional methods.
Pharmacogenomics
Pharmacogenomics enhances personalized medicine by tailoring drug therapies based on an individual's genetic profile, leading to improved efficacy and reduced adverse effects compared to traditional phenotypic data medicine, which relies on observable traits and clinical history. This genetic-centric approach enables precise medication dosing and selection, optimizing treatment outcomes and minimizing the trial-and-error process common in phenotypic-based prescriptions.
N-of-1 Trials
N-of-1 trials in personalized medicine leverage individual genetic and phenotypic data to tailor treatments, enhancing therapeutic efficacy and minimizing adverse effects through precise intervention. Phenotypic data medicine primarily uses observable characteristics to guide treatment but may lack the molecular specificity that personalized approaches provide for optimized patient outcomes.
Multi-omics Integration
Personalized medicine leverages multi-omics integration of genomics, proteomics, metabolomics, and transcriptomics to tailor treatments based on individual molecular profiles, enhancing precision in disease diagnosis and therapy. Phenotypic data medicine complements this by incorporating observable traits and clinical phenotypes, enabling a comprehensive understanding of patient health through the fusion of molecular and phenotypic information.
Genotype-Driven Stratification
Genotype-driven stratification in personalized medicine enables targeted therapies by using patients' genetic profiles to optimize treatment efficacy and minimize adverse effects. Phenotypic data medicine relies on observable traits but lacks the predictive precision that genotype analysis provides for individualized therapeutic strategies.
Longitudinal Phenotypic Profiling
Longitudinal phenotypic profiling captures dynamic health data over time, enabling personalized medicine to tailor treatments based on an individual's evolving physiological and behavioral patterns. This approach contrasts with traditional phenotypic data medicine that often relies on static snapshots, limiting its ability to adapt therapies to real-time patient changes and disease progression.
Integrated Biomarker Panels
Integrated biomarker panels enhance personalized medicine by combining genomic, proteomic, and phenotypic data to deliver tailored treatment strategies that improve patient outcomes. This approach surpasses phenotypic data medicine alone by providing a comprehensive molecular profile for precise disease diagnosis and targeted therapy selection.
Phenome-Wide Association Studies (PheWAS)
Phenome-Wide Association Studies (PheWAS) leverage large-scale phenotypic data to explore associations between genetic variants and a broad spectrum of diseases, enhancing precision in Phenotypic Data Medicine. This approach contrasts with Personalized Medicine's gene-centric focus by integrating diverse phenotypes, enabling more comprehensive insights into complex traits and multifactorial conditions for targeted therapeutic strategies.
Personalized Medicine vs Phenotypic Data Medicine Infographic
 industrydif.com
industrydif.com