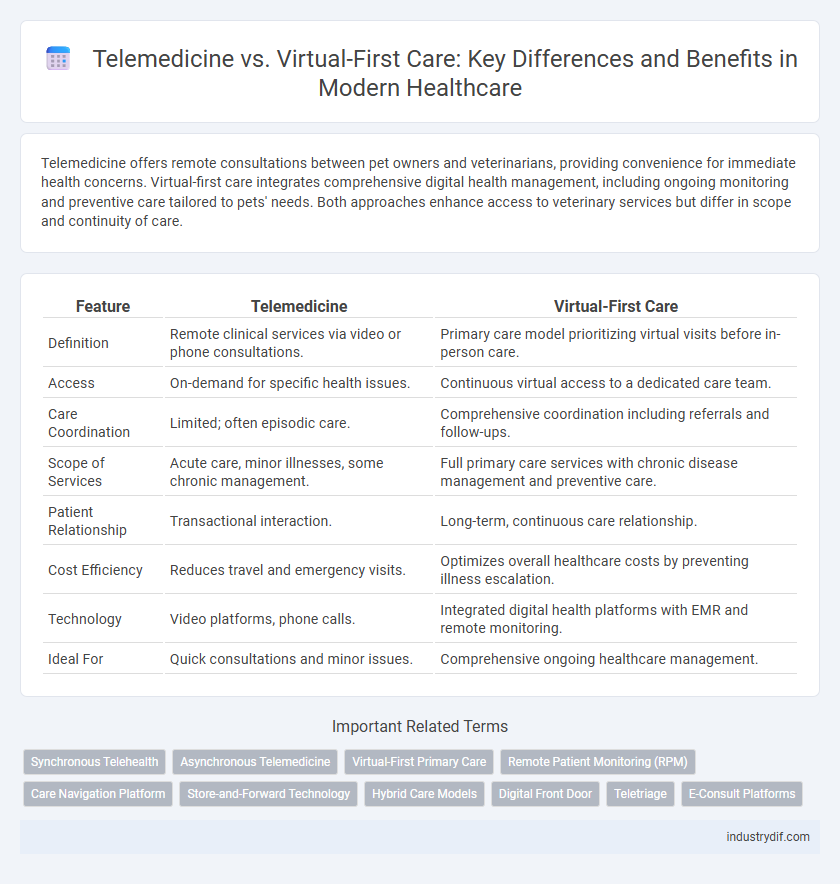
Telemedicine offers remote consultations between pet owners and veterinarians, providing convenience for immediate health concerns. Virtual-first care integrates comprehensive digital health management, including ongoing monitoring and preventive care tailored to pets' needs. Both approaches enhance access to veterinary services but differ in scope and continuity of care.
Table of Comparison
| Feature | Telemedicine | Virtual-First Care |
|---|---|---|
| Definition | Remote clinical services via video or phone consultations. | Primary care model prioritizing virtual visits before in-person care. |
| Access | On-demand for specific health issues. | Continuous virtual access to a dedicated care team. |
| Care Coordination | Limited; often episodic care. | Comprehensive coordination including referrals and follow-ups. |
| Scope of Services | Acute care, minor illnesses, some chronic management. | Full primary care services with chronic disease management and preventive care. |
| Patient Relationship | Transactional interaction. | Long-term, continuous care relationship. |
| Cost Efficiency | Reduces travel and emergency visits. | Optimizes overall healthcare costs by preventing illness escalation. |
| Technology | Video platforms, phone calls. | Integrated digital health platforms with EMR and remote monitoring. |
| Ideal For | Quick consultations and minor issues. | Comprehensive ongoing healthcare management. |
Understanding Telemedicine and Virtual-first Care
Telemedicine uses secure video, phone, or app-based platforms to provide remote clinical services, enabling patients to access healthcare without visiting physical facilities. Virtual-first care prioritizes digital health interactions as the primary mode of patient engagement, often integrating continuous remote monitoring, AI-driven diagnostics, and real-time health data analytics. Both models enhance convenience, reduce healthcare costs, and improve access, but virtual-first care emphasizes a comprehensive digital approach to ongoing health management beyond episodic consultations.
Key Differences Between Telemedicine and Virtual-first Care
Telemedicine primarily delivers remote clinical services through video or phone consultations, while virtual-first care integrates these interactions into a comprehensive digital health model emphasizing continuous patient engagement and proactive management. Telemedicine often serves as an on-demand solution for episodic care, whereas virtual-first care offers broader access to virtual health resources including preventive, chronic, and specialty care. Key differences include care continuity, digital health integration, and focus on preventative versus reactive health management.
Benefits of Telemedicine in Modern Healthcare
Telemedicine enhances patient access by enabling remote consultations, reducing travel time and healthcare costs. It supports timely diagnosis and treatment through real-time video interactions, improving outcomes for chronic disease management and acute care. Integration with electronic health records (EHR) streamlines patient data sharing, fostering coordinated care and personalized treatment plans.
Advantages of Virtual-first Care Models
Virtual-first care models enhance accessibility by offering patients immediate, convenient access to healthcare providers through digital platforms, reducing the need for in-person visits. These models optimize resource allocation, allowing healthcare systems to manage patient flow more effectively and lower overall costs. Patient outcomes improve due to continuous monitoring, personalized care plans, and increased engagement facilitated by integrated digital health tools.
Patient Experience: Telemedicine vs Virtual-first Care
Telemedicine offers patients access to healthcare through scheduled video or phone consultations, reducing travel time but often requiring separate in-person visits for tests or procedures. Virtual-first care integrates digital tools and continuous remote monitoring, providing a seamless, comprehensive experience that prioritizes convenience and proactive management. Patient satisfaction tends to be higher with virtual-first care due to personalized, on-demand support and streamlined access to providers.
Clinical Outcomes: Comparing Effectiveness
Telemedicine and virtual-first care both enhance access to healthcare services, but differences in clinical outcomes are notable. Studies indicate virtual-first care models, which prioritize remote consultations as the initial point of contact, often achieve higher patient adherence and improved management of chronic conditions compared to traditional telemedicine. Data from randomized controlled trials demonstrate virtual-first care can reduce hospital readmissions and emergency visits, emphasizing its effectiveness in continuous, proactive disease management.
Integration with In-person Care Pathways
Telemedicine offers remote consultations that complement in-person care by enabling timely access to specialists and routine follow-ups without geographic constraints. Virtual-first care integrates seamlessly with physical appointments through coordinated electronic health records (EHRs) and real-time data sharing, ensuring continuity and comprehensive management of chronic conditions. This hybrid model optimizes patient outcomes by balancing convenience with critical hands-on diagnostics and treatments.
Technology Platforms and Accessibility
Telemedicine relies on video conferencing platforms and secure messaging systems to connect patients with healthcare providers, emphasizing real-time interactions and accessibility for remote or underserved populations. Virtual-first care integrates advanced digital health platforms that combine telehealth, AI-driven diagnostics, and continuous remote monitoring, offering a proactive and seamless patient experience. Both models leverage mobile apps and cloud-based technologies, but virtual-first care prioritizes comprehensive digital engagement and streamlined access to diverse healthcare services.
Regulatory and Reimbursement Considerations
Telemedicine regulations vary by state and often require providers to adhere to specific licensing and prescribing rules, which can limit cross-state service delivery. Virtual-first care models benefit from evolving reimbursement policies that increasingly recognize continuous remote patient engagement and chronic disease management. Payers and policymakers are gradually expanding coverage for virtual-first programs, reflecting a shift toward value-based care and improved access.
Future Trends in Digital Healthcare Delivery
Telemedicine and virtual-first care are transforming the future of digital healthcare delivery by improving accessibility and patient engagement through real-time video consultations and integrated health platforms. Advances in artificial intelligence, remote monitoring devices, and 5G connectivity are enhancing diagnostic accuracy and enabling personalized treatment plans in virtual settings. Health systems increasingly adopt hybrid models combining in-person and virtual care to optimize outcomes and reduce costs while addressing healthcare disparities globally.
Related Important Terms
Synchronous Telehealth
Synchronous telehealth enables real-time video or phone consultations, providing immediate access to healthcare professionals and facilitating accurate diagnosis and treatment. Virtual-first care often integrates asynchronous tools but relies heavily on synchronous telehealth for urgent and complex health issues requiring direct patient-provider interaction.
Asynchronous Telemedicine
Asynchronous telemedicine enables patients to receive medical consultations and diagnostic evaluations without real-time interaction, enhancing accessibility and convenience compared to virtual-first care models that often rely on live video visits. This approach leverages secure messaging and recorded video to allow healthcare providers to review patient information at their convenience, improving efficiency and expanding timely access to specialty care.
Virtual-First Primary Care
Virtual-first primary care prioritizes remote consultations, offering patients immediate access to healthcare providers through digital platforms, thereby reducing the need for in-person visits and enhancing chronic disease management. This model integrates telemedicine with continuous patient monitoring and proactive care coordination, improving outcomes and lowering healthcare costs compared to traditional telemedicine services focused solely on episodic care.
Remote Patient Monitoring (RPM)
Remote Patient Monitoring (RPM) enhances telemedicine by continuously collecting vital health data, enabling timely clinical decisions without in-person visits. Virtual-first care integrates RPM into a proactive healthcare model, prioritizing remote management to reduce hospital admissions and improve chronic disease outcomes.
Care Navigation Platform
Telemedicine offers on-demand remote consultations through video or phone, while virtual-first care integrates continuous monitoring and proactive health management within a Care Navigation Platform. This platform leverages AI-driven algorithms to streamline patient pathways, optimize resource allocation, and enhance personalized care coordination.
Store-and-Forward Technology
Store-and-Forward technology enables telemedicine by securely transmitting patient data, such as images and medical records, to specialists for asynchronous review, improving access and efficiency in remote diagnostics. Virtual-first care models leverage this technology to reduce wait times and enhance multidisciplinary collaboration without the need for immediate patient presence.
Hybrid Care Models
Hybrid care models integrate telemedicine and virtual-first care to enhance patient access and continuity by combining in-person visits with digital consultations. This approach leverages real-time data sharing and remote monitoring, improving chronic disease management and reducing hospital readmissions.
Digital Front Door
Telemedicine offers on-demand remote consultations primarily for reactive care, while virtual-first care integrates a Digital Front Door strategy that streamlines patient access through pre-visit digital triage, appointment scheduling, and continuous health monitoring. Utilizing advanced AI-powered platforms, the Digital Front Door enhances patient engagement, reduces administrative burden, and ensures seamless navigation across care services.
Teletriage
Teletriage in telemedicine streamlines patient assessment by using digital tools to prioritize care based on symptom severity before in-person visits. Virtual-first care integrates teletriage within its framework, enabling immediate remote evaluation and directing patients to appropriate health services, enhancing efficiency and reducing unnecessary ER visits.
E-Consult Platforms
E-consult platforms streamline healthcare delivery by enabling direct communication between patients and healthcare providers, reducing the need for in-person visits and expediting diagnosis and treatment. Virtual-first care prioritizes remote consultations, integrating telemedicine tools to offer continuous, accessible care while e-consult platforms specifically facilitate specialist advice and collaboration through asynchronous communication.
Telemedicine vs Virtual-first care Infographic
 industrydif.com
industrydif.com