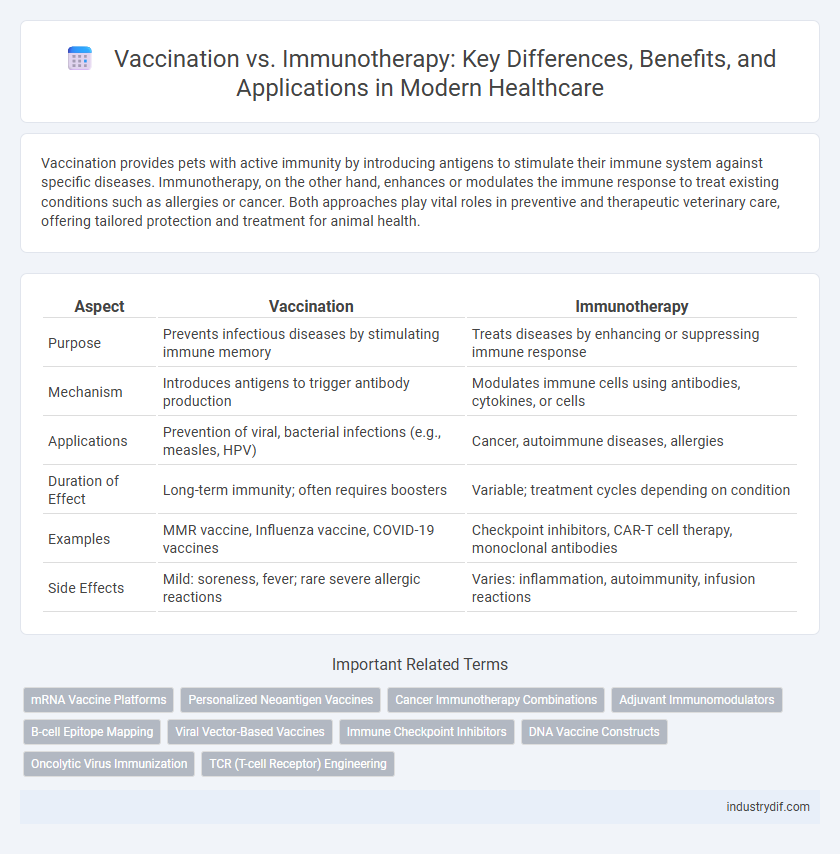
Vaccination provides pets with active immunity by introducing antigens to stimulate their immune system against specific diseases. Immunotherapy, on the other hand, enhances or modulates the immune response to treat existing conditions such as allergies or cancer. Both approaches play vital roles in preventive and therapeutic veterinary care, offering tailored protection and treatment for animal health.
Table of Comparison
| Aspect | Vaccination | Immunotherapy |
|---|---|---|
| Purpose | Prevents infectious diseases by stimulating immune memory | Treats diseases by enhancing or suppressing immune response |
| Mechanism | Introduces antigens to trigger antibody production | Modulates immune cells using antibodies, cytokines, or cells |
| Applications | Prevention of viral, bacterial infections (e.g., measles, HPV) | Cancer, autoimmune diseases, allergies |
| Duration of Effect | Long-term immunity; often requires boosters | Variable; treatment cycles depending on condition |
| Examples | MMR vaccine, Influenza vaccine, COVID-19 vaccines | Checkpoint inhibitors, CAR-T cell therapy, monoclonal antibodies |
| Side Effects | Mild: soreness, fever; rare severe allergic reactions | Varies: inflammation, autoimmunity, infusion reactions |
Understanding Vaccination: Mechanisms and Benefits
Vaccination works by introducing antigens or attenuated pathogens to stimulate the immune system, enabling the body to recognize and combat specific infectious agents more effectively. The primary benefit of vaccination lies in its ability to provide long-lasting immunity, preventing diseases such as measles, influenza, and hepatitis. This proactive approach not only reduces the incidence of infections but also contributes to herd immunity, protecting vulnerable populations.
What Is Immunotherapy? Types and Clinical Applications
Immunotherapy is a groundbreaking treatment modality that harnesses the body's immune system to target and eliminate diseases, including cancer, autoimmune disorders, and allergies. Major types include checkpoint inhibitors, monoclonal antibodies, cancer vaccines, and adoptive cell transfer, each designed to enhance immune response or restore immune function. Clinical applications span oncology, where immune checkpoint inhibitors treat melanoma and lung cancer, to autoimmune diseases and allergen desensitization, showcasing immunotherapy's versatile potential beyond traditional vaccination strategies.
Key Differences Between Vaccination and Immunotherapy
Vaccination primarily aims to prevent infectious diseases by stimulating the immune system to recognize and combat pathogens through antigen exposure. Immunotherapy, on the other hand, treats existing conditions such as cancer or autoimmune diseases by modulating or enhancing the immune response to target abnormal cells or regulate immune activity. While vaccines provide immunity before disease onset, immunotherapy serves as a therapeutic intervention after disease development.
Historical Evolution of Vaccination and Immunotherapy
Vaccination dates back to Edward Jenner's 1796 smallpox vaccine, marking the inception of preventive medicine by introducing weakened pathogens to stimulate immunity. Immunotherapy evolved significantly in the 20th century with advances such as monoclonal antibodies and checkpoint inhibitors, revolutionizing targeted cancer treatments and autoimmune disease management. Both fields reflect a trajectory from empirical experimentation to precision medicine, enhancing disease prevention and personalized therapeutic approaches.
How Vaccines Stimulate Immune Memory
Vaccines stimulate immune memory by introducing antigens that mimic pathogens, prompting the immune system to produce specific antibodies and memory cells without causing disease. These memory B and T cells persist long-term, enabling rapid and robust responses upon future exposures to the actual pathogen. This antigen-specific immune memory distinguishes vaccination from immunotherapy, which often aims to modulate immune responses in existing conditions rather than preventive immunity.
Immunotherapy Strategies in Cancer and Autoimmune Diseases
Immunotherapy strategies in cancer and autoimmune diseases harness the body's immune system to target malignancies or regulate immune responses, employing techniques such as checkpoint inhibitors, CAR T-cell therapy, and monoclonal antibodies. Unlike vaccination, which primarily aims to prevent infections by inducing immunity against specific pathogens, immunotherapy modulates existing immune activity to either enhance tumor destruction or suppress autoimmune reactions. Advances in personalized immunotherapy have improved treatment specificity and efficacy, offering promising outcomes in managing diverse oncological and autoimmune conditions.
Safety Profiles: Vaccination Versus Immunotherapy
Vaccination generally exhibits a well-established safety profile with mild, transient side effects such as soreness or low-grade fever, making it broadly safe for the general population. Immunotherapy, particularly cancer immunotherapy, can lead to more complex immune-related adverse effects including inflammation or autoimmune reactions, requiring careful monitoring. Both modalities necessitate risk-benefit assessment tailored to individual patient conditions, but vaccinations traditionally present fewer severe safety concerns compared to immunotherapy.
Emerging Technologies in Vaccines and Immunotherapeutics
Emerging technologies in vaccines and immunotherapeutics are revolutionizing disease prevention and treatment by enhancing immune system targeting and specificity. Innovations such as mRNA vaccine platforms, nanoparticle delivery systems, and personalized cancer vaccines are crucial for improving immunogenicity and minimizing adverse effects. Advances in bioinformatics and synthetic biology accelerate the design of novel antigens and immune modulators, driving the next generation of precision immunotherapies.
Challenges and Limitations Facing Each Approach
Vaccination faces challenges such as variable efficacy against rapidly mutating pathogens and limited protection duration, necessitating booster doses. Immunotherapy encounters limitations including high costs, potential severe immune-related adverse effects, and complex patient-specific responses that complicate treatment standardization. Both approaches demand ongoing research to enhance safety, effectiveness, and accessibility in diverse populations.
Future Trends: Integrating Vaccination and Immunotherapy
Future trends in healthcare indicate a promising integration of vaccination and immunotherapy to enhance immune system responses against diseases such as cancer and infectious pathogens. Combining the antigen-specific targeting capability of vaccines with the immune checkpoint modulation of immunotherapy offers synergistic potential for personalized treatment strategies. Ongoing research focuses on optimizing delivery methods, identifying novel biomarkers, and improving patient-specific efficacy to revolutionize preventive and therapeutic outcomes.
Related Important Terms
mRNA Vaccine Platforms
mRNA vaccine platforms utilize messenger RNA to instruct cells to produce specific antigens, stimulating a targeted immune response primarily used in vaccination against infectious diseases like COVID-19. Immunotherapy, while also engaging the immune system, often involves modulating immune checkpoints or cellular responses to treat conditions such as cancer, making mRNA vaccines a more direct approach for preventive immunity.
Personalized Neoantigen Vaccines
Personalized neoantigen vaccines represent a cutting-edge approach in cancer immunotherapy, targeting tumor-specific mutations to stimulate a tailored immune response that differs from conventional vaccination methods. These vaccines enhance the precision and effectiveness of immunotherapy by exploiting unique neoantigens derived from an individual's tumor, thereby improving treatment outcomes and minimizing off-target effects.
Cancer Immunotherapy Combinations
Cancer immunotherapy combinations enhance treatment efficacy by integrating vaccines that stimulate tumor-specific immune responses with immune checkpoint inhibitors to overcome tumor-induced immune suppression. Clinical trials demonstrate that combining cancer vaccines with therapies like PD-1/PD-L1 inhibitors significantly improves patient survival rates and reduces tumor progression.
Adjuvant Immunomodulators
Adjuvant immunomodulators enhance the efficacy of both vaccination and immunotherapy by stimulating the immune system to generate a stronger and more sustained response against pathogens or cancer cells. These agents optimize antigen presentation and immune activation, improving clinical outcomes in infectious diseases and oncology treatments.
B-cell Epitope Mapping
B-cell epitope mapping identifies specific regions on antigens recognized by antibodies, enhancing both vaccination and immunotherapy strategies by targeting immune responses more precisely. Advances in epitope mapping enable the design of vaccines and immunotherapies that elicit robust B-cell activation, improving efficacy against infectious diseases and cancer.
Viral Vector-Based Vaccines
Viral vector-based vaccines utilize genetically engineered viruses to deliver antigens, triggering a robust immune response without causing disease, making them effective in preventing infectious diseases like COVID-19. Immunotherapy leverages similar viral vectors but focuses on modifying immune cells to target diseases such as cancer, highlighting distinct applications despite shared technology.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors, a form of immunotherapy, enhance the body's immune response by blocking proteins that suppress T-cell activity, contrasting with vaccination which primes the immune system to recognize specific pathogens. This advanced treatment has shown significant success in cancer therapy, particularly in melanoma and non-small cell lung cancer, by restoring immune system ability to target tumor cells effectively.
DNA Vaccine Constructs
DNA vaccine constructs utilize plasmid DNA encoding specific antigens to induce targeted immune responses, offering precise immunotherapy advantages over traditional vaccination methods. These constructs enhance cellular immunity by promoting endogenous antigen expression, leading to improved efficacy in disease prevention and treatment.
Oncolytic Virus Immunization
Oncolytic virus immunization leverages genetically engineered viruses to selectively infect and destroy cancer cells while stimulating a systemic antitumor immune response, differing from traditional vaccination that primarily prevents infectious diseases by inducing specific immunity. This innovative approach in immunotherapy enhances tumor antigen presentation and recruits immune effector cells, offering promising advancements in personalized cancer treatment.
TCR (T-cell Receptor) Engineering
TCR engineering in immunotherapy harnesses genetically modified T-cell receptors to precisely target cancer cells, offering personalized treatment with enhanced specificity compared to traditional vaccination methods. Unlike vaccines that stimulate broad immune responses, TCR-engineered therapies enable direct recognition and elimination of tumor antigens, improving efficacy in combating resistant malignancies.
Vaccination vs Immunotherapy Infographic
 industrydif.com
industrydif.com