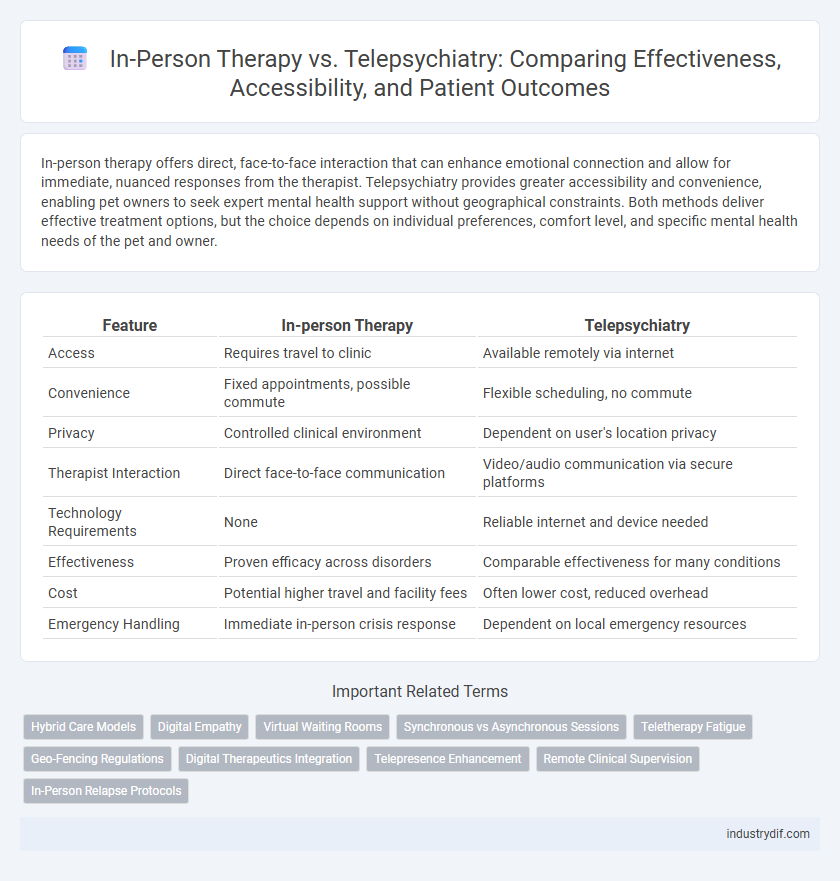
In-person therapy offers direct, face-to-face interaction that can enhance emotional connection and allow for immediate, nuanced responses from the therapist. Telepsychiatry provides greater accessibility and convenience, enabling pet owners to seek expert mental health support without geographical constraints. Both methods deliver effective treatment options, but the choice depends on individual preferences, comfort level, and specific mental health needs of the pet and owner.
Table of Comparison
| Feature | In-person Therapy | Telepsychiatry |
|---|---|---|
| Access | Requires travel to clinic | Available remotely via internet |
| Convenience | Fixed appointments, possible commute | Flexible scheduling, no commute |
| Privacy | Controlled clinical environment | Dependent on user's location privacy |
| Therapist Interaction | Direct face-to-face communication | Video/audio communication via secure platforms |
| Technology Requirements | None | Reliable internet and device needed |
| Effectiveness | Proven efficacy across disorders | Comparable effectiveness for many conditions |
| Cost | Potential higher travel and facility fees | Often lower cost, reduced overhead |
| Emergency Handling | Immediate in-person crisis response | Dependent on local emergency resources |
Definition of In-person Therapy and Telepsychiatry
In-person therapy involves face-to-face sessions between a patient and a mental health professional in a clinical setting, allowing for direct interpersonal interaction and immediate nonverbal communication. Telepsychiatry utilizes digital platforms such as video conferencing to deliver psychiatric assessment, diagnosis, and treatment remotely, expanding access to care for individuals in underserved or remote areas. Both methods aim to provide personalized mental health support, with telepsychiatry leveraging technology to overcome geographical barriers.
Key Differences Between In-person and Virtual Care
In-person therapy offers direct, face-to-face interaction, enabling nuanced body language observation and immediate emotional support, which can enhance therapeutic rapport and effectiveness. Telepsychiatry provides remote access to mental health services through video conferencing, improving convenience and accessibility for individuals in rural or underserved areas while maintaining patient confidentiality. Key differences include the physical presence in in-person sessions that fosters deeper connection versus the flexibility and technology dependence inherent in virtual care.
Benefits of Traditional In-person Therapy
Traditional in-person therapy offers direct, face-to-face interaction, which enhances nonverbal communication cues and emotional connection between patient and therapist. The controlled environment of a therapist's office provides privacy and minimizes distractions, fostering a safe and focused space for mental health treatment. In-person sessions also allow therapists to observe subtle behavioral changes and establish therapeutic rapport more effectively, contributing to personalized care and improved treatment outcomes.
Advantages Offered by Telepsychiatry
Telepsychiatry enhances accessibility by connecting patients with mental health professionals regardless of geographic location, reducing travel time and associated costs. It offers greater scheduling flexibility and privacy, encouraging higher engagement and adherence to treatment plans. Advances in secure video conferencing technology ensure confidentiality while providing real-time, personalized psychiatric care comparable to in-person therapy.
Accessibility and Convenience in Mental Health Services
In-person therapy offers direct human interaction and a controlled environment, enhancing personalized care and immediate emotional support for mental health patients. Telepsychiatry increases accessibility by eliminating geographical barriers and reducing time constraints, enabling individuals in remote or underserved areas to receive professional care conveniently via digital platforms. Both modalities improve mental health service reach, but telepsychiatry excels in flexibility and ease of access for those with mobility or scheduling challenges.
Privacy and Confidentiality Considerations
In-person therapy provides a controlled environment where privacy and confidentiality are easier to maintain, minimizing risks of unauthorized access or data breaches. Telepsychiatry relies on secure, encrypted communication platforms to protect patient information, but potential vulnerabilities in internet connectivity and device security must be managed carefully. Both methods require strict adherence to HIPAA regulations and informed consent protocols to ensure patient confidentiality is upheld.
Clinical Effectiveness and Outcomes
In-person therapy often allows for stronger therapeutic alliance through direct nonverbal cues, which can enhance clinical effectiveness in treating complex mental health disorders. Telepsychiatry has demonstrated comparable outcomes in managing anxiety, depression, and PTSD, offering increased accessibility and convenience for patients. Meta-analyses reveal no significant difference in symptom reduction between modalities, underscoring telepsychiatry as a viable alternative for sustained mental health treatment.
Patient Experience and Satisfaction
In-person therapy provides patients with direct human interaction, fostering a stronger therapeutic alliance and immediate emotional support, which often enhances patient satisfaction. Telepsychiatry offers greater accessibility and convenience, reducing travel time and allowing for flexible scheduling, contributing to positive patient experiences, especially for those in remote areas. Studies show that both modalities yield comparable patient satisfaction rates, but individual preferences and specific conditions play a crucial role in determining the optimal treatment format.
Regulatory and Licensing Challenges
In-person therapy requires therapists to be licensed in the state where the patient is located, creating barriers for cross-state treatment. Telepsychiatry faces complex regulatory challenges due to varying state laws and licensure compacts that limit practice scope and reimbursement. Navigating differing privacy regulations like HIPAA further complicates telepsychiatry implementation compared to traditional in-person therapy settings.
Choosing the Right Approach for Individual Needs
In-person therapy offers direct human interaction and nonverbal cues critical for assessing complex mental health issues, making it ideal for individuals requiring intensive support. Telepsychiatry provides accessible, flexible treatment options, especially beneficial for those in remote areas or with mobility limitations. Selecting between these approaches depends on factors like severity of symptoms, personal comfort with technology, and the need for immediate clinical intervention.
Related Important Terms
Hybrid Care Models
Hybrid care models in mental health integrate in-person therapy and telepsychiatry to enhance accessibility and personalized treatment outcomes. Combining face-to-face sessions with virtual consultations supports continuous monitoring and flexible scheduling, improving patient engagement and reducing barriers to care.
Digital Empathy
Digital empathy in telepsychiatry enhances patient engagement by using video and audio cues to create a sense of presence and understanding comparable to in-person therapy. Advanced platforms leverage AI-driven sentiment analysis to tailor responses, improving emotional connection and treatment outcomes in remote mental health care.
Virtual Waiting Rooms
Virtual waiting rooms in telepsychiatry enhance patient convenience by reducing travel time and allowing seamless session transitions through secure, encrypted platforms optimized for mental health services. These digital environments also support privacy and real-time updates, improving overall therapy accessibility compared to traditional in-person therapy settings.
Synchronous vs Asynchronous Sessions
In-person therapy offers synchronous sessions with real-time interaction that allows immediate verbal and nonverbal cues essential for complex mental health assessments, while telepsychiatry includes both synchronous video calls and asynchronous communication such as messaging or recorded videos, providing flexibility but sometimes limiting immediacy. Studies indicate synchronous telepsychiatry sessions closely replicate traditional therapy outcomes, whereas asynchronous methods are beneficial for ongoing support and tracking but may delay critical interventions in acute cases.
Teletherapy Fatigue
Teletherapy fatigue, characterized by mental exhaustion and decreased engagement during virtual sessions, poses significant challenges for telepsychiatry effectiveness. Factors contributing to this phenomenon include prolonged screen time, limited nonverbal cues, and increased cognitive load, which can diminish therapeutic outcomes compared to traditional in-person therapy.
Geo-Fencing Regulations
Geo-fencing regulations significantly impact the availability and delivery of in-person therapy and telepsychiatry by restricting providers to specific geographic locations, ensuring compliance with state licensing laws and protecting patient privacy. Telepsychiatry platforms must implement precise geo-fencing technology to verify patient locations, enabling legal and secure remote mental health services across state lines while maintaining confidentiality and adherence to HIPAA standards.
Digital Therapeutics Integration
Digital therapeutics integration in telepsychiatry enhances personalized treatment through real-time data analytics and remote monitoring, offering scalable mental health solutions. In-person therapy provides direct human interaction essential for nuanced emotional support, but digital tools complement this by enabling continuous care and adaptive interventions outside clinical settings.
Telepresence Enhancement
Telepsychiatry leverages high-definition video conferencing and real-time data sharing to significantly enhance telepresence, creating an immersive and interactive therapeutic environment that closely mimics in-person sessions. Advanced technologies such as augmented reality (AR) and virtual reality (VR) are increasingly integrated to improve patient engagement, emotional connection, and treatment efficacy in remote mental health care.
Remote Clinical Supervision
Remote clinical supervision enhances telepsychiatry by enabling real-time guidance and oversight for therapists through secure video platforms, ensuring adherence to treatment protocols and improving patient outcomes. In-person therapy relies on direct observation, but telepsychiatry's remote supervision expands access to expert feedback across geographic barriers, facilitating continuous professional development and quality care.
In-Person Relapse Protocols
In-person therapy relapse protocols often involve immediate, personalized intervention, including face-to-face crisis management and real-time observation of nonverbal cues, enhancing accurate assessment and tailored support. These protocols enable therapists to implement structured safety plans and coordinate emergency services promptly, reducing relapse risks more effectively than remote alternatives.
In-person Therapy vs Telepsychiatry Infographic
 industrydif.com
industrydif.com