Monoclonal antibodies target a single specific antigen, providing high specificity and uniformity in therapeutic applications. Bispecific antibodies are engineered to simultaneously bind two different antigens or epitopes, enhancing their ability to recruit immune cells or bring targets into close proximity. This dual targeting increases therapeutic efficacy in complex diseases like cancer by engaging multiple pathways.
Table of Comparison
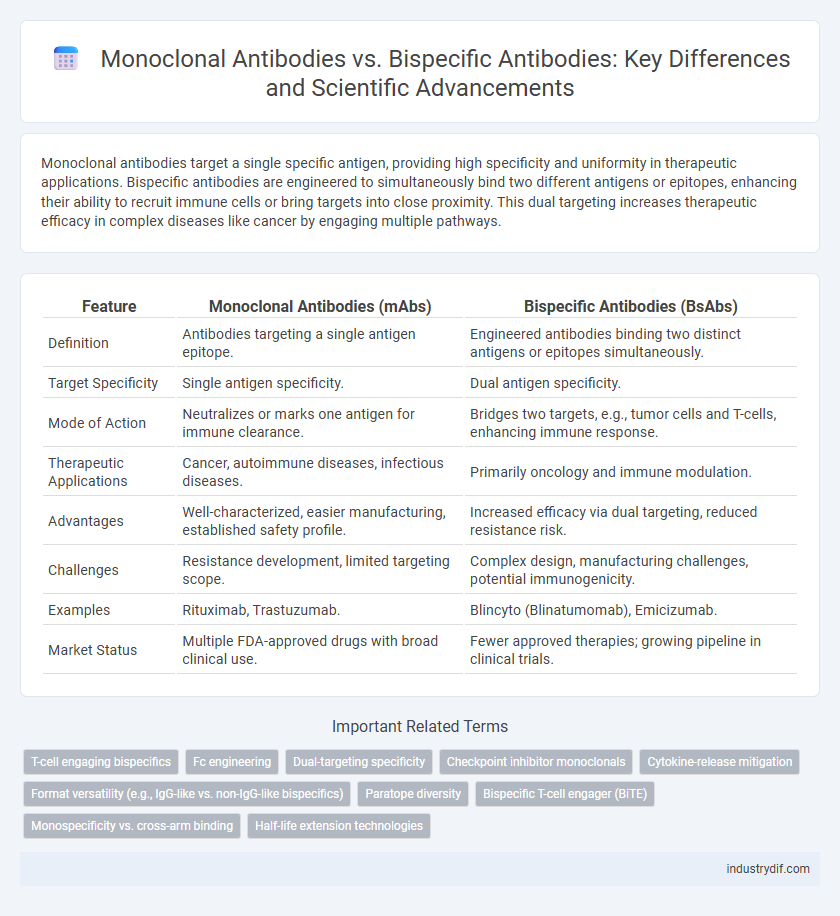
| Feature | Monoclonal Antibodies (mAbs) | Bispecific Antibodies (BsAbs) |
|---|---|---|
| Definition | Antibodies targeting a single antigen epitope. | Engineered antibodies binding two distinct antigens or epitopes simultaneously. |
| Target Specificity | Single antigen specificity. | Dual antigen specificity. |
| Mode of Action | Neutralizes or marks one antigen for immune clearance. | Bridges two targets, e.g., tumor cells and T-cells, enhancing immune response. |
| Therapeutic Applications | Cancer, autoimmune diseases, infectious diseases. | Primarily oncology and immune modulation. |
| Advantages | Well-characterized, easier manufacturing, established safety profile. | Increased efficacy via dual targeting, reduced resistance risk. |
| Challenges | Resistance development, limited targeting scope. | Complex design, manufacturing challenges, potential immunogenicity. |
| Examples | Rituximab, Trastuzumab. | Blincyto (Blinatumomab), Emicizumab. |
| Market Status | Multiple FDA-approved drugs with broad clinical use. | Fewer approved therapies; growing pipeline in clinical trials. |
Overview of Monoclonal and Bispecific Antibodies
Monoclonal antibodies (mAbs) are uniform immunoglobulins derived from a single B-cell clone, designed to specifically target a single antigen epitope with high affinity, widely used in diagnostics and targeted therapy. Bispecific antibodies (BsAbs) are engineered molecules capable of simultaneously binding two distinct antigen epitopes or different antigens, enabling enhanced therapeutic strategies such as redirecting immune cells to tumor cells. The structural diversity of BsAbs, including formats like BiTEs and DARTs, offers improved multifunctionality and therapeutic potential compared to traditional monoclonal antibodies.
Structural Differences Between Monoclonal and Bispecific Antibodies
Monoclonal antibodies consist of two identical heavy chains and two identical light chains forming a Y-shaped structure with uniform antigen-binding sites, while bispecific antibodies are engineered to possess two different antigen-binding sites, enabling simultaneous targeting of distinct epitopes or antigens. The structural complexity of bispecific antibodies often involves various formats such as tandem single-chain variable fragments (scFvs) or dual-variable domain immunoglobulins, which differ fundamentally from the homogenous Fab regions of monoclonal antibodies. These structural differences directly influence their binding specificities, therapeutic applications, and mechanisms of action in immunotherapy.
Mechanisms of Action: Monoclonal vs Bispecific Antibodies
Monoclonal antibodies target a single specific antigen epitope, enabling precise binding and neutralization of pathogens or cancer cells. Bispecific antibodies possess dual binding sites that simultaneously engage two different antigens or epitopes, facilitating cellular recruitment and enhanced immune system activation. This dual-targeting mechanism promotes synergistic therapeutic effects, such as redirecting cytotoxic T cells to tumor cells for improved cancer immunotherapy outcomes.
Therapeutic Applications in Oncology
Monoclonal antibodies (mAbs) selectively target single tumor-associated antigens, enabling precise disruption of cancer cell signaling pathways and immune modulation in oncology therapeutics. Bispecific antibodies (BsAbs) simultaneously bind two different antigens, enhancing immune cell recruitment and tumor specificity, which improves efficacy in complex tumor microenvironments. Clinical studies demonstrate BsAbs offer superior tumor targeting and reduced resistance compared to traditional mAbs in hematologic malignancies and solid tumors.
Manufacturing Challenges and Solutions
Monoclonal antibodies (mAbs) benefit from well-established manufacturing processes, but face challenges such as ensuring consistency and managing glycosylation patterns. Bispecific antibodies introduce additional complexity due to their dual-target binding sites, requiring sophisticated engineering to maintain stability and yield during production. Advances in cell line development and downstream purification technologies are critical solutions improving bispecific antibody manufacturability and scalability.
Pharmacokinetics and Biodistribution Profiles
Monoclonal antibodies (mAbs) exhibit predictable pharmacokinetics characterized by prolonged half-life and stable biodistribution, primarily due to their uniform structure and high affinity for target antigens. Bispecific antibodies (BsAbs) demonstrate altered pharmacokinetics with faster clearance rates and variable tissue penetration, influenced by their dual-target binding and increased molecular complexity. The distinct biodistribution profiles of BsAbs enable simultaneous engagement of two antigens, enhancing therapeutic efficacy but requiring careful optimization to balance target accessibility and systemic exposure.
Clinical Efficacy: Comparative Outcomes
Monoclonal antibodies (mAbs) exhibit targeted therapeutic effects by binding to a single epitope, resulting in well-characterized clinical efficacy across various diseases such as cancer and autoimmune disorders. Bispecific antibodies (bsAbs) simultaneously engage two distinct antigens or epitopes, enhancing clinical outcomes by promoting synergistic mechanisms like improved immune cell recruitment and dual-pathway inhibition. Comparative studies demonstrate that bsAbs often achieve superior response rates and overcome resistance seen with mAbs, although safety profiles and immunogenicity remain critical considerations in clinical applications.
Safety Profiles and Adverse Events
Monoclonal antibodies (mAbs) typically exhibit a well-characterized safety profile, with adverse events such as infusion reactions, cytokine release syndrome, and immunogenicity being relatively manageable. Bispecific antibodies (bsAbs), designed to engage two distinct antigens or epitopes simultaneously, often present a more complex safety landscape, including increased risks of cytokine storm, off-target effects, and higher immunotoxicity due to their dual-specific targeting. Comparative clinical data indicate bsAbs require meticulous dose optimization and monitoring to mitigate severe adverse events while maintaining therapeutic efficacy.
Regulatory Considerations for Antibody Therapies
Monoclonal antibodies (mAbs) and bispecific antibodies (bsAbs) present distinct regulatory challenges due to their structural complexity and mechanism of action. Regulatory agencies require comprehensive characterization of bsAbs to address potential issues like off-target effects, immunogenicity, and stability, which are more pronounced than in conventional mAbs. Approval pathways emphasize rigorous pharmacokinetic and toxicological evaluations to ensure the safety and efficacy of these therapies in clinical applications.
Future Trends in Antibody Engineering
Future trends in antibody engineering emphasize enhanced specificity and multifunctionality, with bispecific antibodies gaining prominence due to their ability to simultaneously target two distinct antigens. Advances in protein engineering and computational modeling enable the design of antibodies with improved binding affinities and reduced immunogenicity. Emerging technologies such as CRISPR and AI-driven algorithms are accelerating the development of next-generation monoclonal and bispecific antibodies for personalized medicine and complex disease treatment.
Related Important Terms
T-cell engaging bispecifics
T-cell engaging bispecific antibodies simultaneously bind to CD3 on T-cells and tumor-associated antigens, enabling targeted cytotoxicity that monoclonal antibodies cannot directly mediate. This dual specificity enhances immune synapse formation and promotes efficient T-cell activation and tumor cell lysis, resulting in improved therapeutic efficacy against cancers.
Fc engineering
Fc engineering in monoclonal antibodies primarily enhances effector functions such as antibody-dependent cellular cytotoxicity and serum half-life through modifications like Fc glycosylation and amino acid substitutions. In contrast, bispecific antibodies require tailored Fc designs to maintain structural stability and dual specificity while optimizing immune effector engagement without compromising target binding.
Dual-targeting specificity
Monoclonal antibodies exhibit high specificity by targeting a single antigen epitope, enabling precise therapeutic action in diseases such as cancer and autoimmune disorders. Bispecific antibodies enhance dual-targeting specificity by simultaneously binding two distinct antigens or epitopes, improving therapeutic efficacy through mechanisms like tumor cell recruitment and immune cell engagement.
Checkpoint inhibitor monoclonals
Checkpoint inhibitor monoclonal antibodies such as pembrolizumab and nivolumab target specific immune checkpoints like PD-1 to enhance T-cell activation against tumors, while bispecific antibodies simultaneously engage two distinct antigens, often merging checkpoint inhibition with direct tumor targeting to improve therapeutic efficacy. The dual specificity of bispecific checkpoint inhibitors allows for localized immune modulation and reduced off-target effects, offering a promising advancement over traditional monoclonal antibody therapies in cancer immunotherapy.
Cytokine-release mitigation
Monoclonal antibodies (mAbs) typically target a single antigen, which can lead to cytokine release syndrome (CRS) due to immune cell overactivation, whereas bispecific antibodies (BsAbs) are engineered to simultaneously engage two distinct antigens, enhancing therapeutic specificity and reducing CRS risk. Advances in BsAb design, such as affinity tuning and selective T-cell engagement, have demonstrated improved cytokine-release mitigation compared to conventional mAbs, optimizing safety profiles in immunotherapy.
Format versatility (e.g., IgG-like vs. non-IgG-like bispecifics)
Monoclonal antibodies typically exhibit a consistent IgG-like format, providing uniform structure and established pharmacokinetics, whereas bispecific antibodies demonstrate format versatility, encompassing both IgG-like and non-IgG-like designs that enable simultaneous targeting of two distinct antigens with varied structural configurations. This versatility in bispecific antibody formats enhances therapeutic potential by facilitating tailored mechanisms of action, improved tissue penetration, and optimized effector functions in diverse clinical applications.
Paratope diversity
Monoclonal antibodies exhibit a single paratope specificity, targeting one distinct epitope on an antigen, which limits their ability to engage multiple pathways simultaneously. Bispecific antibodies possess dual paratopes capable of binding two different epitopes or antigens, enhancing therapeutic efficacy by facilitating complex immune responses and increasing targeting versatility.
Bispecific T-cell engager (BiTE)
Bispecific T-cell engagers (BiTEs) represent a novel class of bispecific antibodies that simultaneously bind to a tumor-associated antigen and CD3 on T-cells, facilitating targeted cytotoxic T-cell activation and tumor cell lysis. Compared to traditional monoclonal antibodies, BiTEs enhance immune synapse formation and promote more efficient and specific T-cell-mediated immunotherapy in hematological malignancies and solid tumors.
Monospecificity vs. cross-arm binding
Monoclonal antibodies exhibit monospecificity by targeting a single antigen epitope, enabling precise immune responses against specific pathogens or cancer cells. Bispecific antibodies possess cross-arm binding capabilities, allowing simultaneous recognition of two distinct antigens, which enhances therapeutic efficacy through recruitment of immune effector cells or dual pathway inhibition.
Half-life extension technologies
Monoclonal antibodies typically rely on Fc engineering and PEGylation to enhance half-life by improving FcRn binding and reducing renal clearance, whereas bispecific antibodies often incorporate albumin-binding domains or fusion partners to simultaneously extend serum half-life and retain multi-target specificity. Advances in half-life extension technologies for bispecific antibodies aim to balance prolonged systemic exposure with maintained functional avidity towards dual antigens, optimizing therapeutic efficacy and pharmacokinetics.
Monoclonal Antibodies vs Bispecific Antibodies Infographic
 industrydif.com
industrydif.com