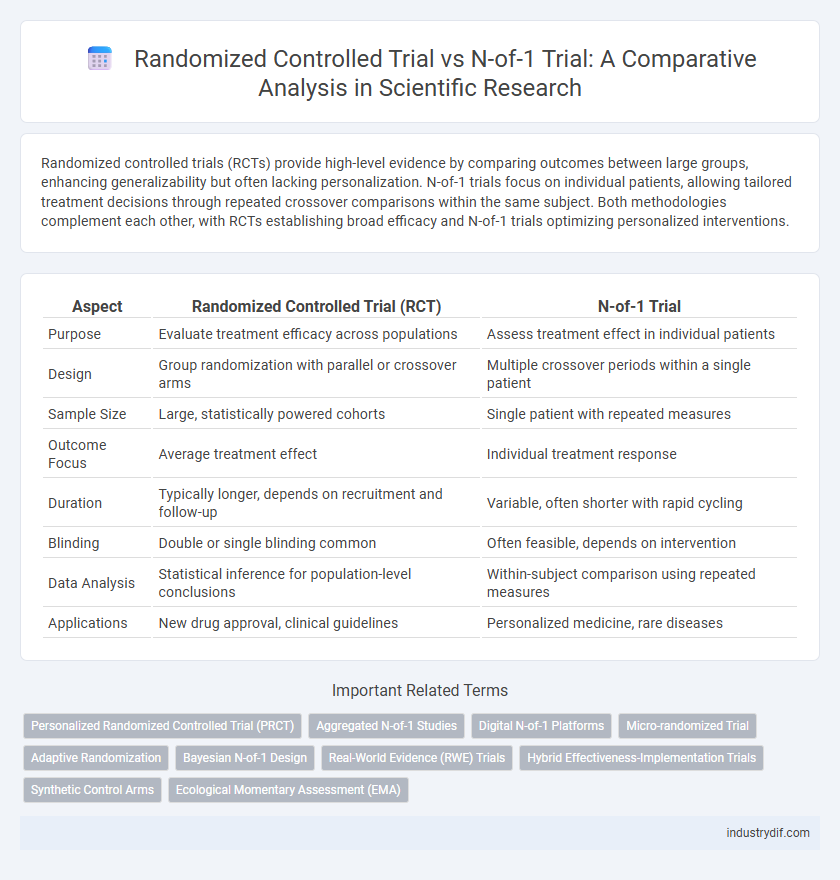
Randomized controlled trials (RCTs) provide high-level evidence by comparing outcomes between large groups, enhancing generalizability but often lacking personalization. N-of-1 trials focus on individual patients, allowing tailored treatment decisions through repeated crossover comparisons within the same subject. Both methodologies complement each other, with RCTs establishing broad efficacy and N-of-1 trials optimizing personalized interventions.
Table of Comparison
| Aspect | Randomized Controlled Trial (RCT) | N-of-1 Trial |
|---|---|---|
| Purpose | Evaluate treatment efficacy across populations | Assess treatment effect in individual patients |
| Design | Group randomization with parallel or crossover arms | Multiple crossover periods within a single patient |
| Sample Size | Large, statistically powered cohorts | Single patient with repeated measures |
| Outcome Focus | Average treatment effect | Individual treatment response |
| Duration | Typically longer, depends on recruitment and follow-up | Variable, often shorter with rapid cycling |
| Blinding | Double or single blinding common | Often feasible, depends on intervention |
| Data Analysis | Statistical inference for population-level conclusions | Within-subject comparison using repeated measures |
| Applications | New drug approval, clinical guidelines | Personalized medicine, rare diseases |
Introduction to Randomized Controlled Trials (RCTs)
Randomized Controlled Trials (RCTs) are considered the gold standard for evaluating the efficacy of medical interventions due to their ability to minimize bias through random allocation of participants to treatment or control groups. By controlling confounding variables and ensuring comparability between groups, RCTs provide robust evidence on treatment effects in diverse populations. The design's strength lies in its capacity to generate generalizable results, making it essential for clinical guideline development and regulatory approvals.
Overview of N-of-1 Trials in Clinical Research
N-of-1 trials represent a personalized approach in clinical research, offering individualized evidence by repeatedly administering treatments to a single patient under controlled conditions. These trials enable precise assessment of treatment efficacy and tolerability, particularly in chronic or rare diseases where traditional randomized controlled trials (RCTs) may lack feasibility or relevance. By focusing on single-patient outcomes, N-of-1 trials enhance personalized medicine through tailored therapeutic decisions and improved patient-centered care.
Key Differences Between RCTs and N-of-1 Trials
Randomized controlled trials (RCTs) involve large populations to assess the efficacy of interventions through random allocation and control groups, producing generalizable results with high statistical power. N-of-1 trials focus on individual participants using multiple crossover periods to determine personalized treatment effects, enhancing precision in patient-specific care. Key differences include sample size, focus on population versus individual outcomes, and methodological design tailored to group inference versus individualized decision-making.
Methodological Design: RCTs vs. N-of-1 Trials
Randomized controlled trials (RCTs) utilize large sample sizes with random allocation to intervention or control groups to ensure statistical power and generalizability, focusing on population-level efficacy. N-of-1 trials, involving repeated crossover of treatments within a single patient, emphasize individual response measurement and personalized treatment optimization. Methodologically, RCTs prioritize between-subject comparisons while N-of-1 trials focus on within-subject variability and treatment effect consistency.
Applicability in Personalized Medicine
Randomized controlled trials (RCTs) provide robust population-level evidence but often lack individual-specific insights crucial for personalized medicine. N-of-1 trials offer tailored data by repeatedly testing treatments within a single patient, enabling more precise therapeutic decisions. Integrating N-of-1 trials in personalized medicine enhances treatment efficacy by adapting interventions to individual variability and response patterns.
Statistical Considerations and Data Analysis
Randomized controlled trials (RCTs) employ group-level statistical analyses such as intention-to-treat and mixed-effects models to assess treatment efficacy and minimize confounding variables. N-of-1 trials utilize within-subject designs, relying on repeated measures and time-series analysis to detect individual treatment effects and intra-subject variability. Statistical power in RCTs is driven by sample size, whereas N-of-1 trials emphasize precision of individual outcome estimates through robust crossover designs and appropriate washout periods.
Strengths and Limitations of Each Trial Type
Randomized controlled trials (RCTs) offer high internal validity and generalizability by minimizing bias through randomization and large sample sizes, but they can be costly and time-consuming with limited applicability to individual patient care. N-of-1 trials provide personalized treatment assessments and adaptability to patient-specific responses, enhancing precision medicine, yet their findings have limited external validity and are resource-intensive for repeated crossover measurements. Balancing these strengths and limitations is essential for optimizing clinical research design and patient-centered outcomes.
Ethical Implications in Trial Selection
Randomized controlled trials (RCTs) offer robust evidence by minimizing bias through randomization but may raise ethical concerns when withholding potentially effective treatments from control groups. N-of-1 trials provide personalized, patient-centered data while maintaining ethical integrity by allowing participants to receive both experimental and control interventions sequentially. Selecting trial designs requires careful consideration of patient autonomy, risk-benefit balance, and the necessity for generalizable versus individualized evidence.
Use Cases: When to Choose RCTs or N-of-1 Trials
Randomized controlled trials (RCTs) are ideal for evaluating population-level intervention efficacy, especially in heterogeneous patient groups requiring broad generalizability and regulatory approval. N-of-1 trials excel in personalized medicine settings, enabling individualized treatment optimization by comparing treatments within the same patient under controlled conditions. Selecting between RCTs and N-of-1 trials depends on research objectives, with RCTs addressing average treatment effects and N-of-1 trials targeting patient-specific responses.
Future Directions in Evidence-Based Research
Future directions in evidence-based research emphasize integrating Randomized Controlled Trials (RCTs) with N-of-1 trials to enhance personalized medicine and optimize treatment efficacy. Advances in digital health technologies and real-time data analytics facilitate the scalability and precision of N-of-1 trials, potentially transforming individualized care pathways. Combining population-level insights from RCTs with patient-specific outcomes from N-of-1 trials offers a robust framework for tailored therapeutic decision-making.
Related Important Terms
Personalized Randomized Controlled Trial (PRCT)
Personalized Randomized Controlled Trials (PRCTs) integrate individual patient characteristics into randomized designs, enhancing precision and treatment efficacy compared to traditional Randomized Controlled Trials (RCTs) that generalize findings across populations. PRCTs address the limitations of N-of-1 trials by maintaining randomization and control while tailoring interventions, thereby optimizing personalized medicine with robust statistical validity.
Aggregated N-of-1 Studies
Aggregated N-of-1 trials combine individual patient-level data from multiple single-patient crossover studies to enhance the statistical power and generalizability of personalized treatment effects compared to traditional randomized controlled trials (RCTs). This approach enables precise estimation of treatment efficacy within heterogeneous populations by integrating variability across individual responses, offering a robust alternative for evidence synthesis in precision medicine.
Digital N-of-1 Platforms
Digital N-of-1 platforms facilitate personalized treatment evaluation by leveraging continuous data collection and real-time analytics, offering greater individual-level precision compared to traditional randomized controlled trials (RCTs), which emphasize population-level efficacy and statistical generalizability. These platforms enable adaptive trial designs and rapid hypothesis testing within a single patient, enhancing the scalability and applicability of precision medicine interventions in clinical practice.
Micro-randomized Trial
Micro-randomized trials (MRTs) differ from traditional randomized controlled trials (RCTs) and N-of-1 trials by randomizing interventions repeatedly within individuals over time to assess proximal treatment effects. These trials are particularly effective for evaluating just-in-time adaptive interventions by capturing dynamic changes in behavior and context at a fine-grained temporal resolution.
Adaptive Randomization
Adaptive randomization in randomized controlled trials (RCTs) dynamically modifies allocation probabilities based on interim outcomes to enhance treatment efficacy detection and ethical balance. In contrast, N-of-1 trials employ individualized crossover designs without adaptive randomization, optimizing personalized treatment by repeated measurements within a single patient.
Bayesian N-of-1 Design
Bayesian N-of-1 trials utilize adaptive statistical models to analyze individual patient data, enhancing personalized treatment decisions compared to traditional randomized controlled trials (RCTs) that assess average effects across populations. This design allows continuous updating of posterior probabilities, providing tailored therapeutic insights and increasing the efficiency of clinical interventions at the individual level.
Real-World Evidence (RWE) Trials
Randomized controlled trials (RCTs) provide high internal validity by comparing interventions across large populations, whereas N-of-1 trials offer personalized insights through repeated crossover testing within a single patient, enhancing real-world applicability. Real-World Evidence (RWE) trials leverage data from routine clinical practice, with N-of-1 designs capturing individual responses and RCTs generalizing findings to broader populations, thereby complementing each other in evidence generation.
Hybrid Effectiveness-Implementation Trials
Hybrid effectiveness-implementation trials combine the rigorous methodology of randomized controlled trials (RCTs) with the personalized approach of N-of-1 trials to evaluate both clinical outcomes and implementation processes simultaneously. This integrated design enhances the applicability of findings by assessing individual patient responses while facilitating real-world adoption of interventions.
Synthetic Control Arms
Randomized controlled trials (RCTs) provide robust data through population-level comparisons, while N-of-1 trials offer personalized evidence by evaluating individual patient responses over time; synthetic control arms leverage real-world or historical data to augment or replace traditional control groups, enhancing trial efficiency and ethical feasibility. Integrating synthetic control arms in RCTs or N-of-1 designs improves statistical power and reduces patient recruitment burdens by creating well-matched, data-driven comparators without randomization.
Ecological Momentary Assessment (EMA)
Randomized controlled trials (RCTs) provide robust population-level evidence but often lack ecological validity, whereas N-of-1 trials integrate Ecological Momentary Assessment (EMA) to capture real-time, individualized data reflecting daily fluctuations in symptoms and behaviors. The application of EMA within N-of-1 trials enhances personalized treatment optimization by continuously monitoring context-specific responses, thereby improving internal validity and external generalizability in precision medicine.
Randomized controlled trial vs N-of-1 trial Infographic
 industrydif.com
industrydif.com